On this page
These guidelines were published in 2019 and are awaiting review, due 2022. Some content may be outdated.
Indications
- High clinical risk of fetal growth restriction (maternal hypertensive disease, pre‑eclampsia, maternal smoking, IVF, previous FGR/SGA, maternal medical disease) or as per the Growth Assessment Protocol (GAP)
- Current FGR, SGA or reduced interval fetal growth (see the SGA guideline (PDF, 2.9 MB) for more detail, NZMFMN 2014a and Appendix 9: SGA scanning schedule) (section 88 codes: GR and GF)[1]
- Diabetes (NIDDM, IDDM, gestational diabetes)
- Placental location (code: PL)
- Malpresentation (code: MP)
- Antepartum haemorrhage (code: AH)
- Abdominal pain (code: AP)
- Reduced fetal movements (code: FC)
- Follow up for fetal abnormality (see below), for example, renal dilatation – see also Appendix 7: Fetal renal tract dilation charts
- Maternal red cell antibodies/Rhesus incompatibility (see below)
- Spontaneous or preterm premature rupture of membranes (see below)
- Polyhydramnios/oligohydramnios (see below)
- Multiple pregnancy (see Multiple Pregnancy [PDF, 318 KB], NZMFMN 2015f).
Note: A growth scan is not recommended in women where symphysial-fundal height (SFH) is tracking along or above the 90th centile if gestational diabetes has been excluded and there is no clinical concern regarding polyhydramnios (see the SGA guideline (PDF, 2.9 MB) for more detail, NZMFMN 2014a).
[1] See Appendix 1: Ultrasound scan codes and indications.
Note: In the absence of any clinical indications, routine post-date scanning is not currently recommended.
Required clinical details
- Reason for scan/symptoms, as per section 88 indication
- EDD based on earliest scan, if available
- Relevant history
- Previous caesarean section(s).
Third-trimester ultrasound examination
Fetal biometry
Growth charts as per local protocol. At present, ASUM are used in most sites.
- BPD
- HC
- AC
- FL
- Estimated fetal weight (EFW) (Hadlock A) or Shepard (AC and FL) if accurate head measurements cannot be obtained.
As per the SGA guideline (PDF, 2.9 MB) and Obstetric Doppler guideline (PDF, 3.7 MB) (NZMFMN 2014a and 2014b respectively), suboptimal fetal growth is suspected when:
- AC ≤5th centile on population chart
- AC centile smaller than head by ≥30 centiles
- AC >5th centile but dropping by ≥30 centiles
- change in AC of <5 mm over 14 days
- EFW <10th centile on customised chart (eg, GROW)
- EFW dropping by ≥30 centiles on customised chart.
The minimum interval between growth scans is 14 days. See Appendix 9: SGA scanning schedule.
- Fetal number
- Fetal lie and position
- Fetal cardiac activity
- Gestational age
- Placenta – location in relation to the cervix
- Placenta accreta: where there is anterior placenta previa and previous caesarean section, the overlying myometrium should be carefully assessed using high resolution TA and TV scanning with some fluid within bladder
- Amniotic fluid (see below)
- Doppler (only if indicated, see Doppler chapter)
- Maternal adnexa (only if indicated, see Abdominal pain below)
- Limited fetal anatomy (see Fetal anatomy below).
Amniotic fluid
- Measurement to include amniotic fluid index (AFI) and single deepest pocket.
- AFI varies with gestation (plot on a standardised chart).
- Normal deepest pocket is between 2 and 8 cm.
- Polyhydramnios is defined as single deepest pocket of ≥10 cm and/or AFI ≥25 cm.
- Oligohydramnios is defined as single deepest pocket <2 cm.
Doppler
Routine Doppler is not indicated.
For more detail, see the SGA guideline (PDF, 2.9 MB) and Obstetric Doppler guideline (PDF, 3.7 MB) (NZMFMN 2014a and 2014b respectively) for Doppler indications and the Doppler chapter.
Fetal anatomy
This assessment is for uncomplicated scans performed after 20 weeks, assuming a previous normal anatomy scan.
For otherwise uncomplicated serial scans, detailed assessment of anatomy is only necessary once in the third trimester.
For the first scan in the third trimester, image:
- ventricle / choroid plexus – measure if abnormal
- 4Ch heart, including IVS (+ colour)
- 3VT / arrow view (+ colour)
- both kidneys (measure AP pelvis in trans if dilated)
- bladder
- stomach
- lips/nose.
Fetal wellbeing (interval amniotic fluid and Doppler) scan
If growth assessment as above has been performed within the last two weeks, a limited fluid and Doppler scan may be indicated, particularly as directed by the SGA pathway (see Appendix 9).
Ultrasound examination
- Fetal lie
- Amniotic fluid assessment as above
- Doppler (if indicated, see Doppler chapter)
- Fetal stomach and bladder
- Document fetal movements.
Third-trimester scan for other indications
Ultrasound examination
Routine assessment as per Third-trimester ultrasound examination above, with additional views as below.
Diabetes in pregnancy
The recommended frequency of scans for women with gestational diabetes is outlined in Screening, Diagnosis and Management of Gestational Diabetes in New Zealand: A clinical practice guideline (Ministry of Health 2014).
Assessment of IVS in diabetes
An increase in fetal IVS and ventricular wall thickness is reported in diabetic pregnancy. These babies are at increased risk of cardiomyopathy. Consider measurement of the IVS in diabetic patients with EFW ≥90th centile.
IVS imaging technique
- Orientate transducer so the beam is perpendicular to the long axis of the heart.
- Measure peri-membranous portion of IVS either with M-mode or B-mode.
- Measure during diastole (when AV valves are open).
- Measure at tip of AV valves.
- Plot figure obtained on standardised chart if available.
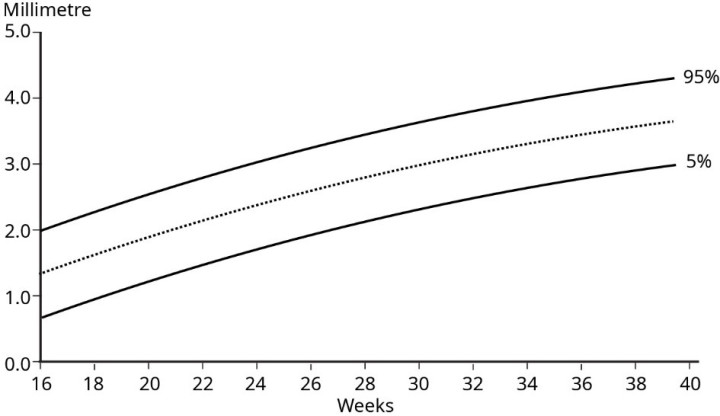
Figure 3: IVS imaging technique
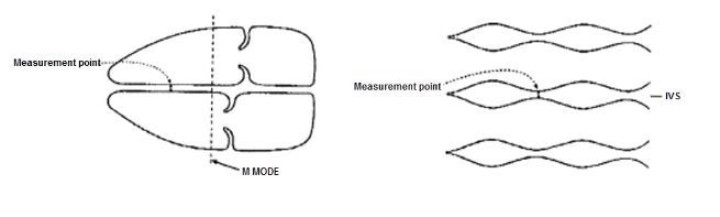
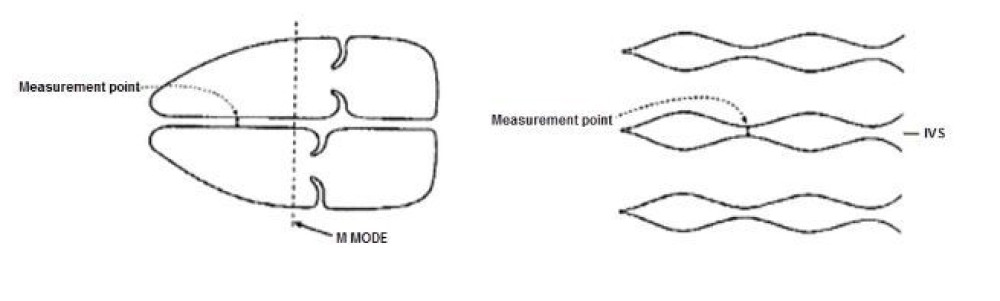
Source: Canterbury DHB Obstetric and Gynaecology Ultrasound Protocols, June 2019 (internal DHB document).
Figure 4: IVS reference chart
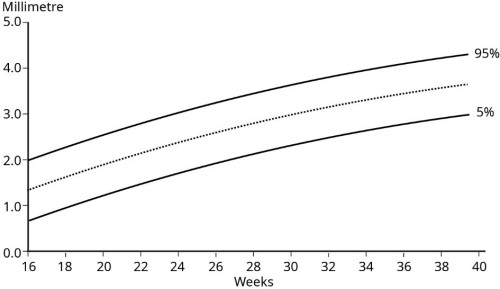
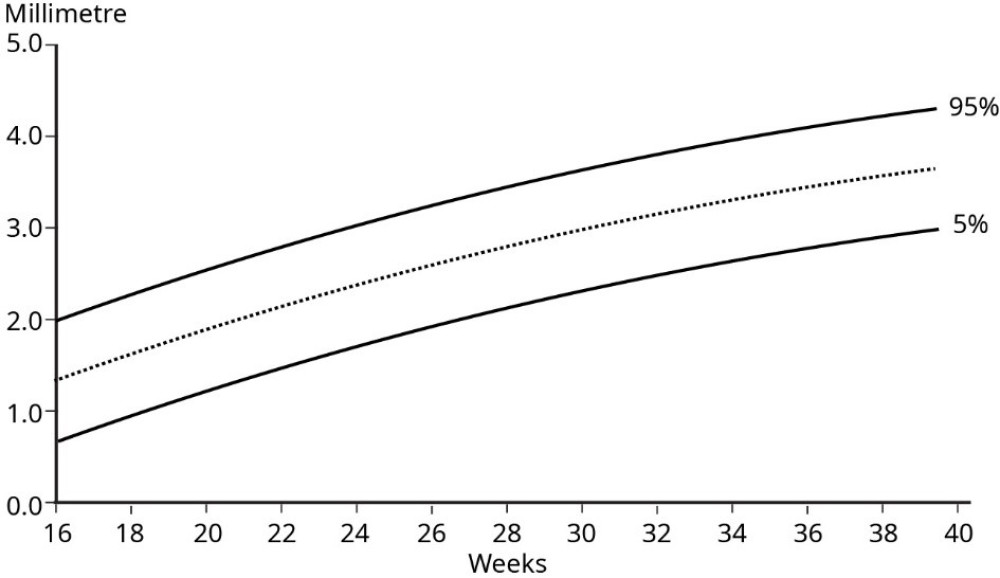
Source: Tan et al 1992.
Maternal antibodies involved in haemolytic disease of the newborn, for example, Rhesus incompatibility
- If there are known maternal antibodies, perform MCA PSV and plot on the appropriate graph. See New Zealand Obstetric Doppler Guideline (PDF, 3.7 MB) (NZMFMN 2014b). These women should be under specialist care.
- Specialist referral is required for PSV >1.5 MoM.
- Assess for fetal hydrops – identification of hydrops should prompt immediate discussion with the referrer to arrange urgent Fetal Medicine or specialist referral.
Antepartum haemorrhage
- Ultrasound should not be requested in cases of strong clinical suspicion of abruption as this is a clinical emergency.
- Document placental location, structure, cord insertion and distance of lower placental margin from internal cervical os. Consider use of colour for further evaluation of retroplacental haemorrhage/abruption.
- Routine colour box over internal cervical os to exclude vasa previa.
- TV scan should be considered if:
- the lower placental margin is not clearly seen on TA scan
- the placenta is low lying or possible previa
- there is a placental anomaly, for example, succenturiate lobe, velamentous or marginal cord insertion.
- TV scanning is generally contraindicated in patients with ruptured or bulging membranes. PV bleeding is not a contraindication for TV scanning.
Abdominal pain
- Placental location and structure – exclude haematoma (consider use of colour for further evaluation of retroplacental haemorrhage/abruption)
- Maternal adnexa/ovaries
- Maternal renal tract if clinically indicated
- Maternal right iliac fossa (RIF) – if clinically appropriate to assess for possible appendicitis
- Maternal upper abdomen / gallbladder – only if requested or specifically indicated, for example, right upper quadrant (RUQ) or epigastric pain
- If maternal renal colic is suspected, or if maternal ureteric dilatation is seen, consider TV scan to assess for a calculus in the distal ureter.
Spontaneous or preterm premature rupture of membranes
- Document amniotic fluid.
- Place colour box over the cervix – helpful if the cervix appears open in order to exclude a prolapsed umbilical cord.
- TV scanning is generally contraindicated in patients with ruptured membranes.
- Note: Ultrasound is not a substitute for clinical diagnosis of preterm premature rupture of the membranes (PPROM).
Polyhydramnios/Oligohydramnios
- Document amniotic fluid.
- For oligohydramnios, consider causes such as: SGA, spontaneous rupture of membranes (SROM) / premature rupture of membranes (PROM), renal anomalies such as obstructive uropathy and bilateral renal abnormality.
- For polyhydramnios, consider causes such as: large for gestational age (LGA), maternal type 2 diabetes mellitus (T2DM), gestational diabetes mellitus (GDM), upper gastrointestinal problem (such as duodenal atresia, oesophageal atresia or trachea-oesophageal fistula), major brain anomaly, facial abnormality.
- For a combination of SGA and polyhydramnios, consider aneuploidy.
Multiple pregnancy
See Twin pregnancy chapter and the guideline Multiple Pregnancy (PDF, 318 KB) (NZMFMN 2015f).
Placenta
- Follow-up for placental location in cases of low-lying placenta detected in the second trimester (section 88 code PL, see Appendix 1) or possible placenta accreta/AIP.
Malpresentation
- Section 88 code MP (see Appendix 1)
- Report position of the fetus, including the presenting part.
Follow-up of fetal renal dilatation or other relevant second-trimester findings
Assess relevant anatomy, for example, fetal renal tract – see Appendix 7: Fetal renal tract dilation charts.
Reduced fetal movements
- Section 88 code FC (see Appendix 1)
- Doppler (umbilical artery Doppler, ± middle cerebral artery if appropriate – see New Zealand Obstetric Doppler Guideline [PDF, 3.7 MB], NZMFMN 2014b)
- Document fetal movements/breathing.
Reporting guide and recommendations
Minimum reporting requirements
- Dating information by previous scan (if available)
- Fetal biometry
- Fetal position/lie
- Placental location and its relation to the cervix
- Amniotic fluid (AFI, deepest pocket)
- Fetal anatomy with structures, as per Third-trimester ultrasound examination (see above)
- Doppler – only if indicated (see the SGA guideline [PDF, 2.9 MB] and Obstetric Doppler guideline [PDF, 3.7 MB], NZMFMN 2014a and 2014b respectively)
- Conclusion regarding interval growth if there has been a previous third-trimester scan
- Recommendation of follow-up scan at an appropriate interval if there is concern regarding growth, amniotic fluid or Doppler as per the SGA guideline.
Scan frequency
See the SGA guideline (PDF, 2.9 MB) (NZMFMN 2014a) and Appendix 9: SGA scanning schedule.
- High-risk pregnancies: 2- to 3-week scan interval, for example, for monochorionic diamniotic (MCDA) twins (see Multiple Pregnancy [PDF, 318 KB], NZMFMN 2015f), previous FGR, pre-eclampsia toxaemia (PET), intrauterine fetal death (IUFD) or reduced interval growth on scan
- Routine: 4-weekly intervals, for example for GDM, dichorionic diamniotic (DCDA) twins demonstrating normal interval growth.
Reporting pro forma
Reporting alerts
Emergency
- Placental abruption
Urgent
- Critically abnormal Doppler
- Hydrops
- Anhydramnios
- PV bleeding in context of accreta
- Absent fetal movements in context of other evidence of fetal distress
Same day
- Abnormal Doppler, eg, elevated umbilical artery Doppler with continuous forward flow
- Mildly reduced MCA pulsatility index and cerebroplacental ratio
- Structural fetal anomaly, unless previously reported and stable.