On this page
Ultrasound examination
These guidelines were published in 2019 and are awaiting review, due 2022. Some content may be outdated.
- Document placental location, for example, anterior, posterior, fundal.
- Ask about any previous caesarean section and document placental location in relation to the scar.
- Image in transverse and longitudinal planes.
- Measure distance of the lower placental margin/marginal sinus from the internal os. Consider a TV scan if the lower margin cannot be well visualised in relation to the internal os.
- A full bladder can simulate low-lying placenta; if in doubt, get the woman to empty her bladder.
- Less than 20 mm is considered low lying. Third-trimester follow-up is recommended.
- Assess placental cord insertion and location.
- In case of velamentous cord insertion, placenta previa or succenturiate lobe, careful assessment of the internal os is required with colour Doppler, with a low threshold for TV imaging, to exclude vasa previa.
Placental anomalies
- Placenta previa / low-lying placenta (see below)
- Velamentous cord insertion
- Marginal cord insertion
- Succenturiate lobe
- Vasa previa (see below)
- Suspected placenta accreta (see below)
- Placental mass, for example, chorioangioma.
Low-lying placenta and placenta previa
The placenta is inserted wholly or partially into the lower segment of the uterus. Terms used to describe types of placenta previa include:
- complete placenta previa – the placenta completely covers the internal cervical os
- partial placenta previa – the placenta is partly over the cervix
- marginal previa – the placenta is near the edge of the cervix
- low-lying placenta – the placenta/marginal sinus is 20 mm or less from the internal cervical os.
Image 3


Complete placenta previa.
Vasa previa
Vasa previa occurs when exposed fetal vessels within the amniotic membranes cover, or are within 20 mm of, the internal cervical os.
This is a clinically significant condition as the vessels are from the fetoplacental circulation, and rupture will lead to rapid fetal exsanguination and death.
There are two types of vasa previa.
- Type I occurs with velamentous insertion of the umbilical cord into the placenta.
- Type II occurs with velamentous fetal vessels connecting the placenta to a succenturiate placental lobe.
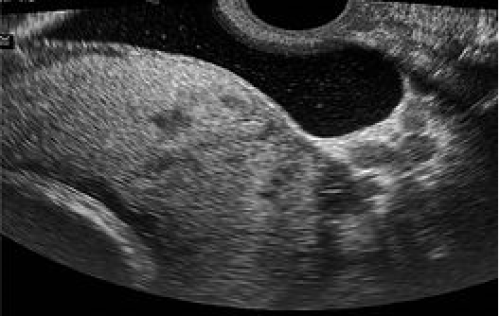
Image 4
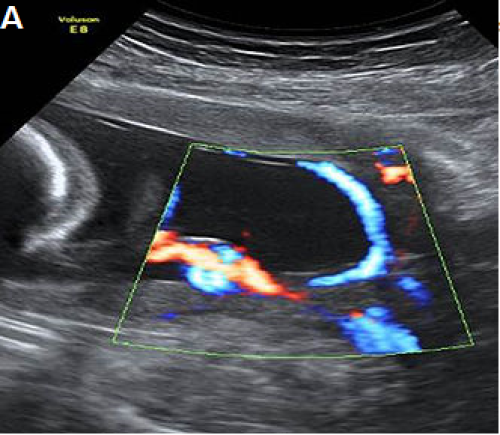
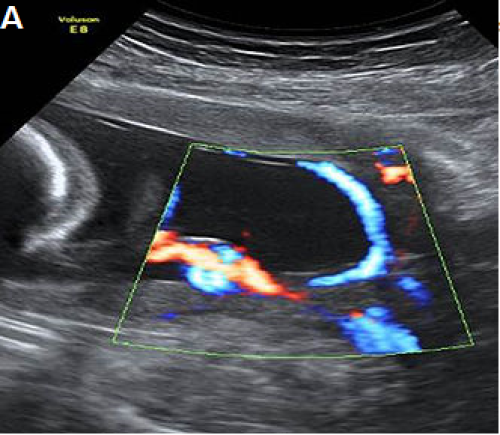
Type I vasa previa, with a velamentous cord insertion and vessels coursing over the internal os.
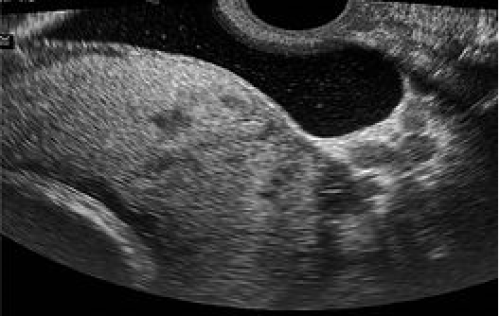
Image 5
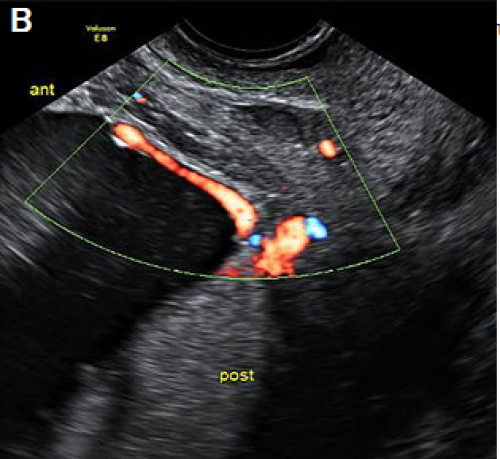
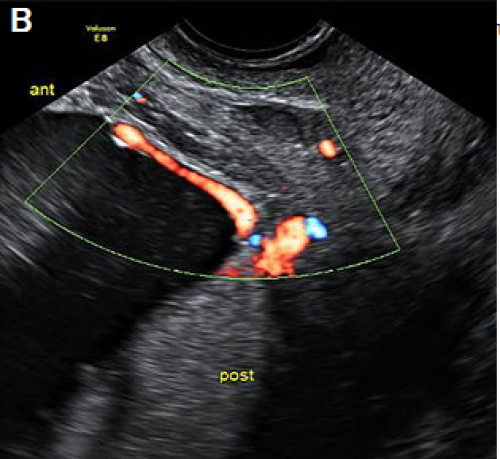
Type II vasa previa, with vessels coursing over the cervix between the main posterior placental lobe and a smaller anterior succenturiate lobe.
Image 6
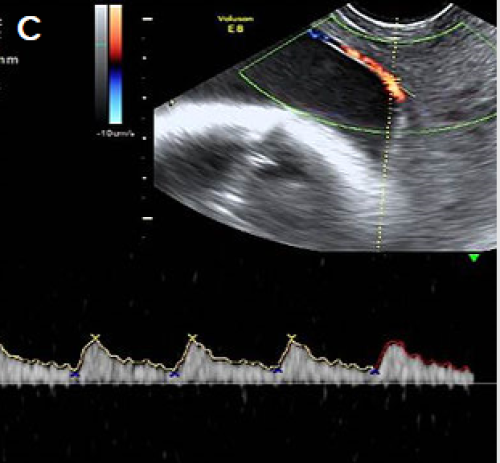
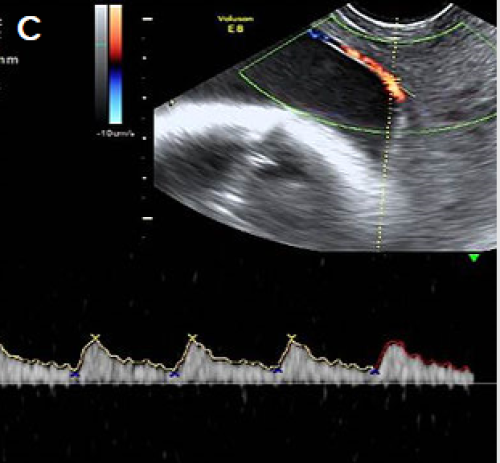
Pulsed Doppler showing a fetal arterial waveform in the vessels crossing the cervix.
For more detail, see The Royal Australian and New Zealand College of Obstetricians and Gynaecologists (RANZCOG) statement Vasa Praevia (PDF, 9.1 MB) (RANZCOG 2016).
Reporting guide and recommendations
If a low-lying placenta and/or placenta previa (see above) is found at the anatomy scan, recommend follow-up at approximately 32 weeks gestation, which may include a TV scan.
If there is evidence of vasa previa (see above) at the anatomy scan, report the finding and recommend specialist review and follow-up scans.
Placenta accreta / abnormally invasive placenta
Placenta accreta / abnormally invasive placenta (AIP) is a disorder of placental implantation where there is invasion of placental tissue into the uterine wall. It is associated with a high risk of maternal and fetal morbidity and mortality.
Careful assessment is recommended with women who have had a previous caesarean section where the placenta overlies the scar, and if there are any concerns, tertiary opinion is recommended.
Traditionally, the extent may be mild, moderate or severe. However, this can be difficult to assess accurately on ultrasound.
- Accreta – placental extension through the thinned decidua basalis without myometrial invasion
- Increta – invasion into the myometrium
- Percreta – invasion through the myometrium with breach of the serosa, with or without invasion into adjacent structures, for example, into the bladder.
The most common risk factors are a previous caesarean section and placenta previa (see above).
Features of abnormal placental implantation include:
- irregular placental lakes/lacunae
- focal bulging of the placenta
- abnormal myometrial-bladder wall interface
- loss of retroplacental hypoechoic space
- disordered vascularity.
For first-trimester features, see Appendix 2: Low gestational sac in the first trimester with previous caesarean section.
Required clinical details
- Parity
- Number of previous caesarean sections
- Number of classical caesarean sections
- Number of previous surgical evacuations (including termination of pregnancy, TOP)
- Previous uterine surgery (eg, myomectomy, endometrial ablation)
- Past history of accreta/AIP.
Ultrasound features
Greyscale features
- Loss of clear zone – loss or irregularity of the hypoechoic retroplacental ‘clear’ zone in the myometrium underneath the placental bed.
- Myometrial thinning overlying the placenta to <1 mm, or undetectable.
- Abnormal placental lacunae – often numerous, including some that are large and irregular, often containing turbulent flow visible on greyscale imaging.
- Bladder wall interruption – loss or interruption of the echogenic bladder wall between the uterine serosa and the bladder lumen.
- Placental bulge – deviation of the uterine serosa away from the expected plane, caused by abnormal bulge of placental tissue into a neighbouring structure, typically the bladder. The uterine serosa appears intact, but the outline is distorted.
- Focal exophytic mass – placental tissue is evident breaking through the uterine serosa and extending beyond it. This is most often seen within the filled bladder.
Colour Doppler ultrasound features
- Uterovesical hypervascularity – striking colour Doppler flow between the myometrium and posterior wall of the bladder.
- Subplacental hypervascularity – striking colour Doppler flow within the placental bed.
- Bridging vessels – vessels extending from the placenta, across the myometrium ± beyond the serosa into the bladder or other organs; these often course perpendicular to the myometrium.
- Placental lacunae feeder vessels – vessels with high-velocity blood flow leading from the myometrium into the placental lacunae, with turbulence.
- Parametrial involvement – suspicion of invasion into the parametrium.
Ultrasound examination
- The lower segment of the uterus should be carefully assessed for possible placenta accreta at the anatomy scan in women who have had previous caesarean sections, placenta previa or both, particularly if the placenta is anterior.
- Pay particular attention to the anterior uterine wall-bladder wall interface.
- Assess with a combination of TV and TA scan with a high-frequency transducer, such as a linear array.
- Consider TV scan with the bladder partially full to provide an interface with the myometrium.
- Longitudinal and transverse images (without and with colour Doppler).
- Assess for above features of AIP.
For more detail, see:
- FIGO consensus guidelines on placenta accreta spectrum disorders: Prenatal diagnosis and screening (Jauniaux et al 2018)
- Proposal for standardized ultrasound descriptors of abnormally invasive placenta (AIP) (Collins et al 2016)
- Pro forma for ultrasound reporting in suspected abnormally invasive placenta (AIP): an international consensus (Alfirevic et al 2016).
Reporting guide
- Report placental location (anterior, posterior) and distance from os.
- Report suspicious ultrasound findings (as at Ultrasound features above).
Recommendations
If there are features suspicious for placenta accreta at the anatomy scan, recommend specialist referral and follow-up detailed scan.
Image 7
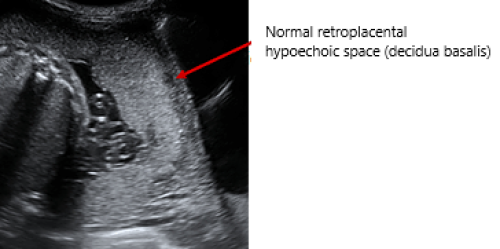
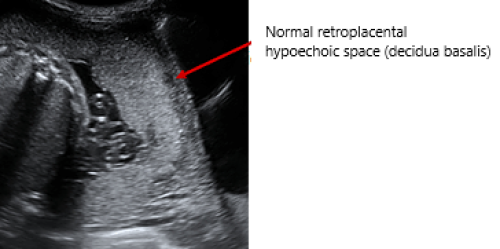
- Sagittal view lower uterine segment and bladder (TA)
- Complete placenta previa
- Normal ‘clear zone’ retroplacental hypoechoic space
- No lacunae
- No evidence of placenta accreta on greyscale imaging.
Image 8


- Sagittal anterior lower uterus and bladder (TA)
- Complete placenta previa
- Loss of clear zone (retroplacental hypoechoic space)
- Irregular large lacunae
- Placental bulge into bladder
- Highly suspicious for placenta accreta on greyscale imaging.
Image 9
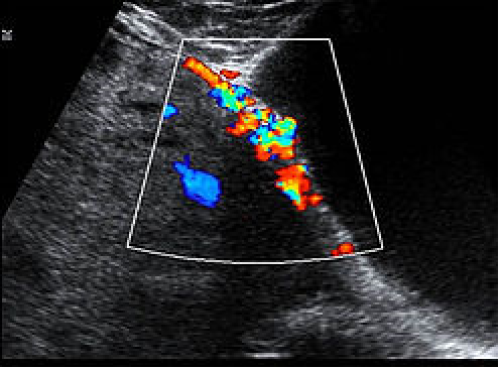
- Sagittal anterior lower uterus and bladder TA with colour Doppler
- Loss of clear zone
- Irregular lacunae
- Uterovesical hypervascularity
- Subplacental hypervascularity
- Bridging vessels
- Suspicion of focal exophytic vascular mass into the bladder
- Highly suspicious for placenta accreta on colour Doppler imaging.
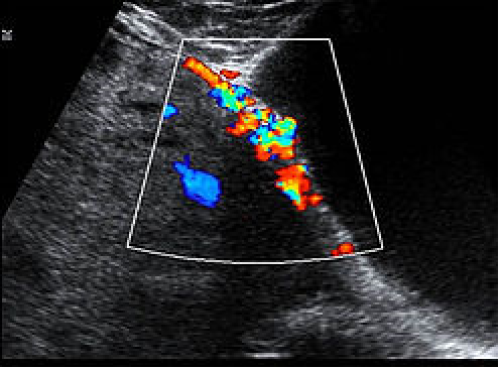
Image 10
- Lower uterine segment and bladder TV with bladder partially filled
- Complete placenta previa
- Loss of clear zone
- Placental bulge
- Placental lacunae
- Highly suspicious for placenta accreta on greyscale imaging.
Image 11
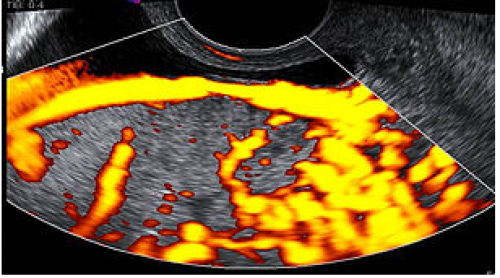
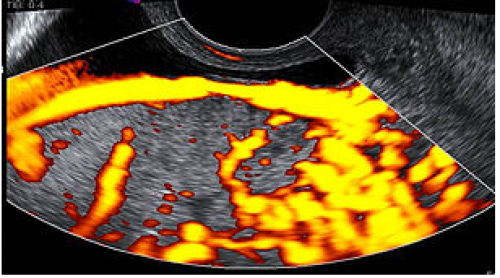
Lower uterine segment and partially filled bladder TV with power Doppler
Complete placenta previa
Loss of clear zone
Marked placental bed hypervascularity
Placental lacunae and feeder vessels
Highly suspicious for placenta accreta on colour Doppler imaging.
- Lower uterine segment and partially filled bladder TV with power Doppler
- Complete placenta previa
- Loss of clear zone
- Marked placental bed hypervascularity
- Placental lacunae and feeder vessels
- Highly suspicious for placenta accreta on colour Doppler imaging.
Reporting alerts
Emergency
- Active bleeding in the setting of vasa or placenta previa or accreta.