On this page
These guidelines were published in 2019 and are awaiting review, due 2022. Some content may be outdated.
Assessment of chorionicity and amnionicity (see below) is vital (first-trimester assessment is optimal).
Label the leading fetus ‘twin A’ and the following fetus ‘twin B’ and record position as left and right and upper and lower, by the relationship of each sac to the cervix, and assign gender if discordant.
Twins frequently change position: the description of fetal position must be clear, and state if the previously leading twin is no longer presenting; however, the labelling of twins A and B must not be changed during the pregnancy.
For further information, see Multiple Pregnancy (PDF, 318 KB) (NZMFMN 2015f).
Ultrasound screening in twins
Dichorionic twins
- 12–13+6 week scan for each fetus as per singleton pregnancy. The NT is used for screening for aneuploidy in twins and is combined with biochemistry to provide a risk assessment.
- Anatomy scan at 19+ weeks.
- Third-trimester scan (growth scans) every four weeks, with the addition of Doppler and fortnightly growth as per the SGA guideline (PDF, 2.9 MB) (NZMFMN 2014a) if either twin meets SGA criteria.
Monochorionic twins
- 12–13+6 week scan for each fetus as per singleton pregnancy. The NT is used for screening for aneuploidy in twins and is combined with biochemistry to provide a risk assessment.
Discordant CRL in monochorionic twins is associated with an increased risk of subsequent development of selective fetal growth restriction (sFGR).
Discordant NT in monochorionic twins may be associated with an increased risk of subsequent development of TTTS.
Because of the potential complications of monochorionic twinning, including TTTS, TAPS and sFGR, fortnightly scans are advised from 16 weeks gestation to delivery.
Every scan must include:
- biometry for both twins including EFW from 20 weeks, amniotic fluid deepest vertical pool for both sacs, presence/absence of bladder and stomach filling
- document UA Doppler from 20 weeks, or before if signs of TTTS or sFGR; assess for normal, absent or reversed end-diastolic flow
- anatomy scan at approximately 20 weeks
- from 24 weeks, MCA PSV in both twins.
In the case of fetal demise of one fetus, there is a significant risk of ischemic brain damage in the surviving co-twin. A Fetal Medicine referral is needed.
Consideration should be given to magnetic resonance imaging (MRI) 6 weeks after the event, or longer depending on the gestation and parental wishes. Note: MRI is a tertiary-level decision.
Diagnosis of TTTS
- Oligohydramnios of one twin with deepest pocket <2 cm and polyhydramnios of the other, deepest pocket >10 cm. If there is discordancy that does not meet these criteria, but the sonographer/radiologist has concerns, recommend referral to local Fetal Medicine unit for a decision on the next scanning or review required.
- Quintero staging (based on discrepancy of amniotic fluid):
Quintero staging
| Stage 1 |
|
|---|---|
| Stage 2 |
|
| Stage 3 |
|
| Stage 4 |
|
There may be associated growth discrepancy and abnormal Doppler.
See Staging of twin-twin transfusion syndrome (Quintero et al 1999).
Diagnosis of TAPS
Raised MCA PSV (>1.5 MoM) indicating fetal anaemia in one twin and MCA PSV <1.0 MoM in the other.
Note: If only one MCA can be ascertained but it is between 1.0 and 1.5 MoM, then there is less concern to achieve the assessment of the second twin.
Diagnosis of sFGR
EFW discordance of >25 percent or EFW of one twin <10th centile.
Weight discordance is calculated as: (EFW larger twin – EFW smaller twin) / EFW larger twin.
Gratacos staging is used for sFGR (types I–III) (Bennasar et al 2017; Gratacos et al 2007).
Referral recommendations
Under the Guidelines for Consultation with Obstetric and Related Medical Services (Referral Guidelines) (Ministry of Health 2012), women with a multiple pregnancy should be under the care of a specialist obstetrician, though in many cases, care is shared with a midwifery LMC.
A specialist with an interest in high-risk pregnancy should be involved in the following situations:
- high-risk first-trimester screening or anomaly on anatomy scan
- amniotic fluid discordancy
- growth discordancy of >20 percent EFW.
Where there are ultrasound signs of TTTS, early referral within 24 hours to the regional Fetal Medicine unit is recommended for further assessment.
This condition can deteriorate quickly, and treatment for severe cases is available only in Auckland.
Reporting alerts
Emergency
- Open cervix
Urgent
- New diagnosis of TTTS
- New diagnosis of significant fetal abnormality
- Critically abnormal Doppler
Same day
- New diagnosis of TAPS
- New diagnosis of sFGR.
Determining chorionicity and amnionicity in twins
Chorionicity should be ascertained and clearly imaged for future reference at the earliest scan possible (ideally ≤14 weeks). If it is too early or not clear, a follow-up scan should be offered.
Dichorionic twins
- Lambda sign (λ) indicates dichorionic diamniotic (DCDA) pregnancy.
- Identification of two separate placentas has a specificity of 100 percent but may not be evident after the first trimester because the placentas often fuse later in gestation.
- Fetuses with different genders are always dizygous and therefore dichorionic.
Image 45
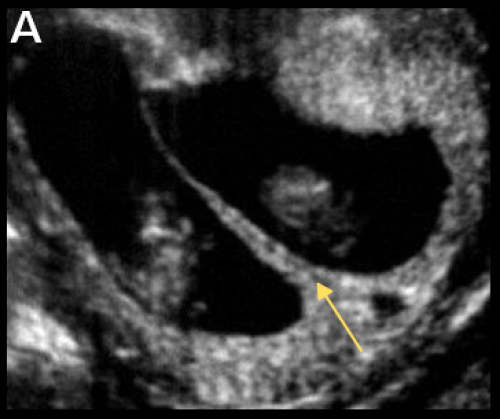
Lambda sign (arrow) indicating DCDA twin pregnancy.
Monochorionic twins
- Tau sign (τ) has a sensitivity of 100 percent and specificity of 98 percent for monochorionic diamniotic (MCDA) pregnancy.
- Thickness of membranes <1.5 mm or lack of Lambda sign suggests MCDA pregnancy.
- Absence of membranes indicates monochorionic monoamniotic (MCMA) pregnancy (confirm with TV scan if possible).
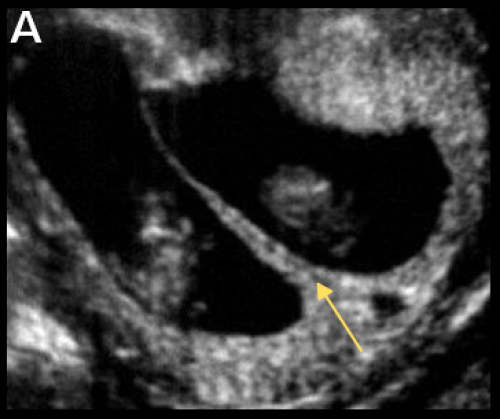
Image 46




T sign (arrow) indicating MCDA twin pregnancy (B) and absent intertwin membrane (C) in a MCMA twin pregnancy.
Dating
- The largest CRL should be used for dating in twin pregnancy, unless IVF / assisted reproduction, in which case the IVF dates (date of intrauterine insemination or ovum pick-up) should be used.
- Ideally, the pregnancy should be dated by CRL between 10+0 and 12+6 weeks gestation.
- After 13 weeks, dating may be performed using mean HC.
Complications in monochorionic twin pregnancies
All twin pregnancies have increased rates of anomaly, preterm birth (both spontaneous and iatrogenic), pre-eclampsia, sFGR, GDM and complicated delivery, but the rate of complications is significantly increased in monochorionic (MC) twinning, due to placental anastomoses.
Twin-to-twin transfusion syndrome
- Occurs in 10–15 percent of MC twin pregnancies.
- Most commonly occurs between 16–26 weeks gestation and if untreated has a perinatal mortality rate of 80–90 percent.
- Due to placental anastomoses, which cause unidirectional flow along connecting vessels – one twin receives more blood flow than the other.
- Has a poor prognosis, leading to up to 20 percent of all perinatal deaths in twins.
- Discordant amniotic fluid volumes are the initial findings.
Twin anaemia-polycythaemia sequence
- Also due to placental anastomoses
- Usually occurs later in pregnancy
- Has a better prognosis
- Characterised by one twin being anaemic and the other polycythaemic, without the discordant amniotic fluid associated with TTTS.
Selective fetal growth restriction
- Common complication of a MC twin pregnancy
- Due to unequal placental sharing
- Can be associated with a poor outcome if it occurs early in pregnancy
- May occur in combination with TTTS and contributes to difficulties in diagnosis and treatment.
Demise of one twin
- Depending on the gestational age at demise, the surviving twin may be affected by increased rates of:
- death of co-twin
- neurologic abnormality (due to ischaemic brain damage)
- preterm delivery.
- Consider MRI for surviving co-twin (this is a tertiary-level decision).
Monoamniotic twins
- Identical twins that share the same sac.
- Very high-risk pregnancy due to:
- cord entanglement
- cord compression
- TTTS – which is difficult to diagnose due to the single sac.
Twin reversed arterial perfusion (TRAP) sequence
- Also known as acardiac twinning.
- Rare, occurring in 1 percent of MC twin pregnancies.
- One twin is usually structurally normal (the ‘pump twin’); the other (‘acardiac twin’) is abnormal, often consisting of a lower body and lower limbs with absent or rudimentary upper body, head and heart.
- Due to abnormal vascular connections between the twins with arterial flow from the umbilical artery of the pump twin into the acardiac twin – illustrated on colour Doppler or pulsed wave ultrasound as reversed arterial perfusion within the abnormal twin.
- The pump/normal twin may develop high output cardiac failure.
- Untreated, mortality of the normal/pump twin approaches 50 percent.
Conjoined twins
- Rare
- Occurs in monoamniotic twins
- Classified by the anatomic site at which the twins’ bodies are joined, most commonly:
- thoraco-omphalopagus – fused from upper chest to lower chest
- thoracopagus – fused from upper thorax to lower abdomen
- omphalophagus – fused at lower abdomen
- craniopagus – fused skulls and separate bodies.