Appendix 6: Placental anomalies
Appendix 6 for the New Zealand Obstetric Ultrasound Guidelines.
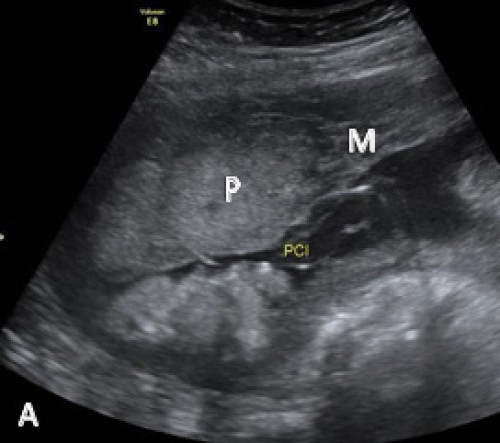
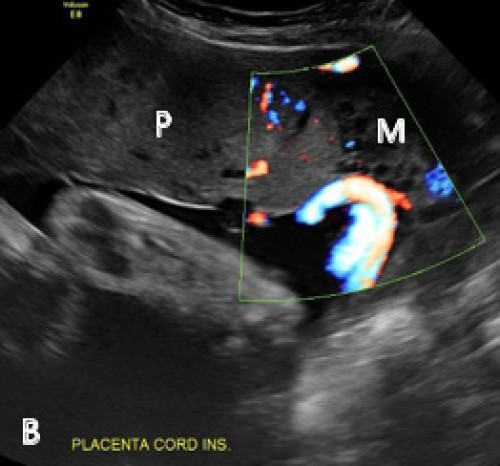
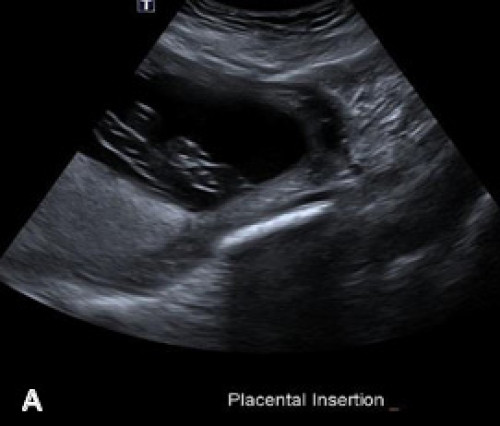
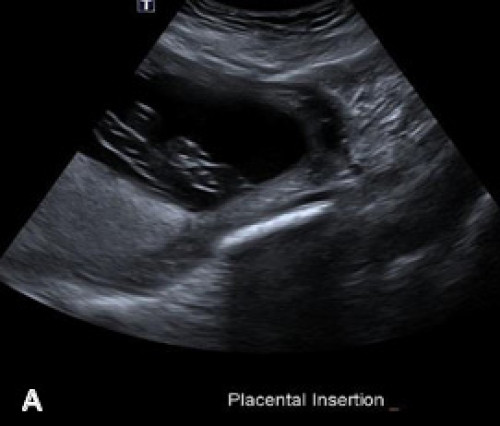
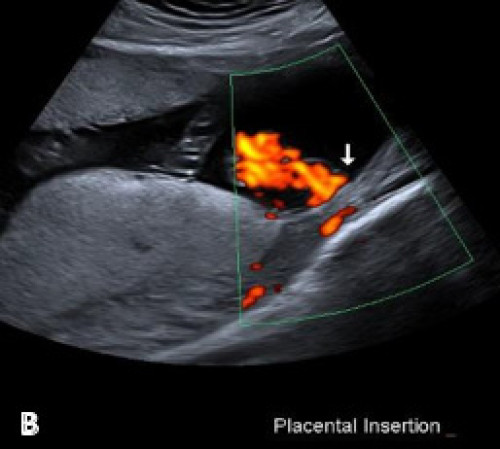
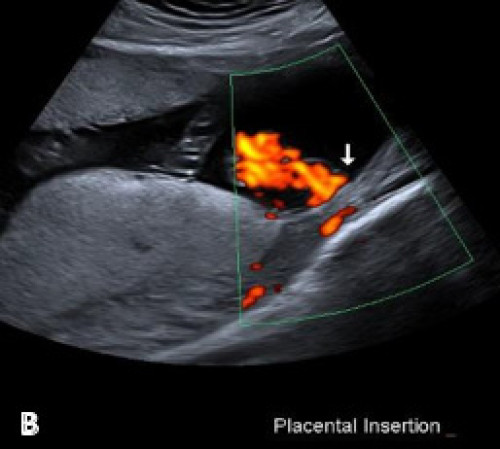
Marginal cord insertion on greyscale (A) and colour Doppler (B) imaging.
Placenta (P), myometrium (M).
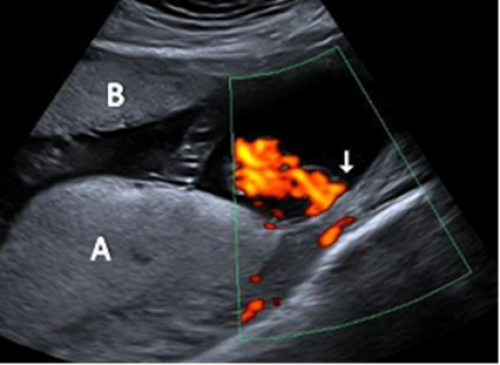
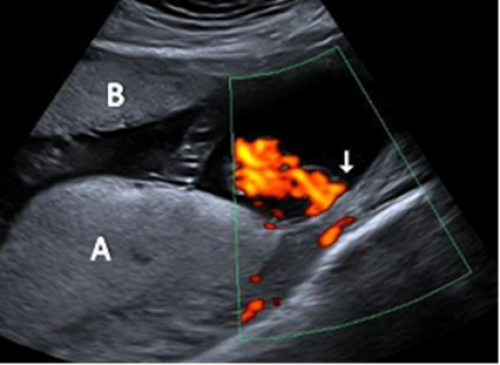
Velamentous cord insertion on greyscale imaging (A) and with colour Doppler (B).
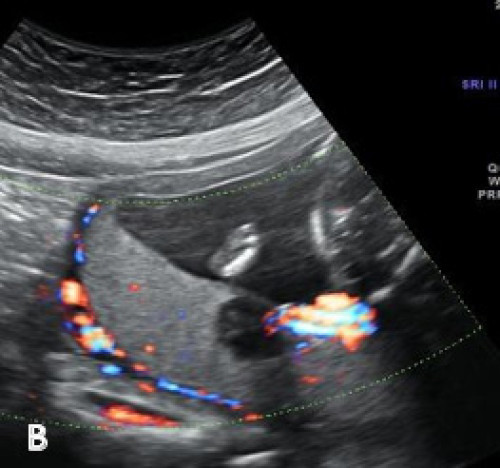
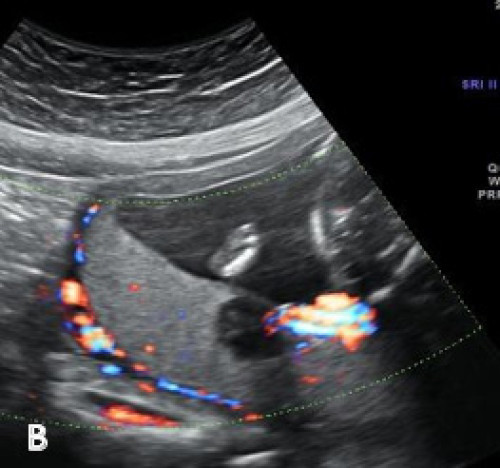
Main placental lobe posteriorly (A) and smaller anterior succenturiate lobe (B), associated with a velamentous cord insertion.


Heterogeneous hypoechoic lesion within the posterior placenta on greyscale imaging (A) and with colour Doppler (B), showing its location adjacent to the placental cord insertion.