On this page
- How are we doing?
- First episode rheumatic fever hospitalisations, annual rate per 100,000 people, New Zealand, 2007/2008–2024/2025
- First episode rheumatic fever hospitalisations, annual rate per 100,000 people, by ethnic group, New Zealand, 2007/2008-2024/2025
- First episode rheumatic fever hospitalisations, annual rate per 100,000 people, by age group, New Zealand, 2024/2025
- First episode rheumatic fever hospitalisations, annual rate per 100,000 people, by Health District of Residence, 2024/2025
- First episode rheumatic fever hospitalisations, annual rate per 100,000 people, by Health Region of Residence, 2024/2025
- Where to from here?
- Rheumatic Fever Report 2024/2025
- Rheumatic Fever Roadmap, 2023-2028
The Roadmap ensures we have a strong focus on eliminating inequities, meeting our commitments to Te Tiriti o Waitangi, ensuring timely access to quality care and placing the needs of people with lived experience of rheumatic fever and rheumatic heart disease at the heart of our efforts.
Data on this page is sourced from the National Minimum Dataset. 2024-2025 data presented includes 1 July 2024 – 30 June 2025.
How are we doing?
In 2024/2025, there were 194 people admitted to hospital for the first time with rheumatic fever (3.62 per 100,000 people) in New Zealand. This number has stayed the same since 2023/2024, with the rate of hospitalisation similar to that experienced in 2018/2019 and returning to pre-COVID-19 levels.
Following a decrease in the rate of first time hospitalisations with rheumatic fever for Māori between years 2011/2012 to 2015/2016, this rate has fluctuated between 5.4 and 8.9 per 100,000 people over the last ten financial years.
First time rheumatic fever hospitalisations for Pacific peoples have fluctuated quite strongly over the period shown below. In 2021/2022 the hospitalisation rate for Pacific peoples was the lowest since 2007/2008. However, over the past three financial years the rates have increased, with the rate in 2024/2025 being comparable to the previous peak in 2018/2019.
The annual number of Non-Māori, Non-Pacific people admitted to hospital with rheumatic fever for the first time is low. The rate of hospitalisation over the relevant period was lowest in 2021/2022 (0.12 per 100,000 people). However, rates for more recent years have been higher (0.4 per 100.000 people in 2024/2025). In 2024/2025, Māori were 18 times more likely to be hospitalised for the first time with rheumatic fever than Non-Māori, Non-Pacific people, while Pacific peoples were almost over 70 times more likely.
An insights report was completed in 2024, which provided analysis of rheumatic fever and rheumatic heart disease through the COVID-19 pandemic in New Zealand. This work was led by Tōmaiora, researchers from the University of Auckland. Key findings included significant decreases in crude acute rheumatic fever hospitalisation rates in 2021-2022, however marked inequities still persisted for Māori and Pacific peoples. The COVID-19 elimination-suppression strategy had a significant independent effect in a best fit model, associated with a reduction in acute rheumatic fever hospitalisations by 50%.
It is not surprising to see an increase in rheumatic fever hospitalisations, given what has occurred with other childhood respiratory infections (viral, invasive pneumococcal disease etc.) during the pandemic, with infection rates initially falling then now rising again. Health New Zealand will continue to watch the situation closely.
It is also important to note that while New Zealand has higher rates of rheumatic fever compared to other development countries, the annual numbers are small. Therefore, changes year-to-year may be real, or they may be an artifact of the variability that is seen when there are small numbers of cases.
First episode rheumatic fever hospitalisations, annual rate per 100,000 people, New Zealand, 2007/2008–2024/2025
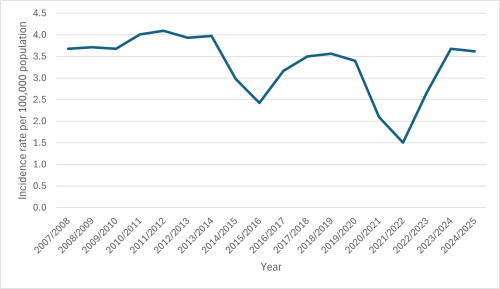
The figure above shows the rate per 100,000 people admitted to hospital with rheumatic fever for the first time from financial years 2007/2008 to 2024/2025.
The figure above shows the rate per 100,000 people admitted to hospital with rheumatic fever for the first time from financial years 2007/2008 to 2024/2025.
First episode rheumatic fever hospitalisations, annual rate per 100,000 people, by ethnic group, New Zealand, 2007/2008-2024/2025
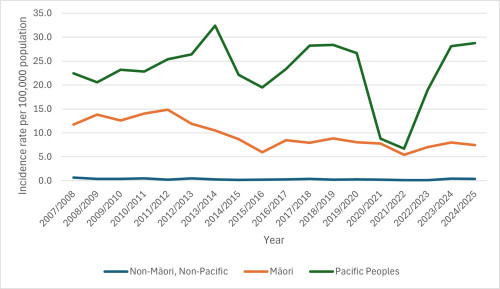
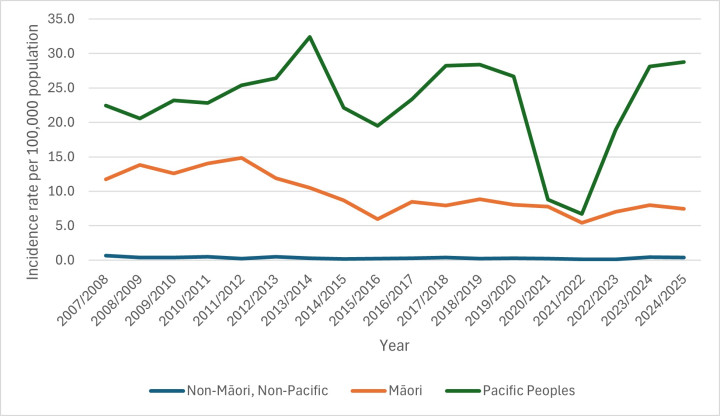
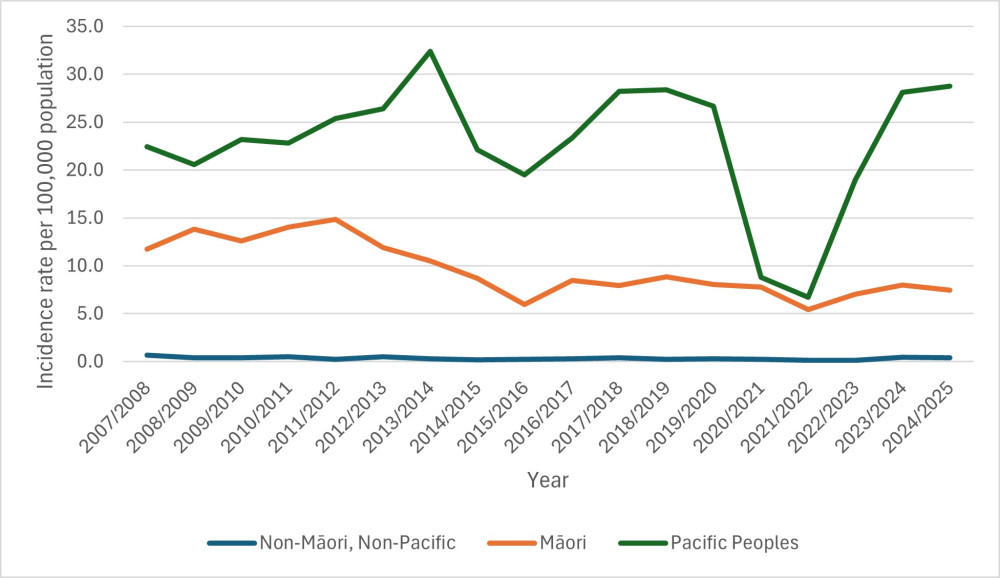
The figure above shows the rate per 100,000 people admitted to hospital with rheumatic fever for the first time from financial years 2007/2008 to 2024/2025 by ethnicity.
The figure above shows the rate per 100,000 people admitted to hospital with rheumatic fever for the first time from financial years 2007/2008 to 2024/2025 by ethnicity.
First episode rheumatic fever hospitalisations, annual rate per 100,000 people, by age group, New Zealand, 2024/2025
The following table shows the numbers and rates of people being admitted to hospital with rheumatic fever for the first time in 2024/2025 by age group. It shows that the majority of cases continue to occur in children between 5 and 14 years (54%).
|
|
Numbers |
Rate per 100,000 |
|
0–4 years |
<10 |
- |
|
5–14 years |
105 |
15.7 |
|
15–24 years |
41 |
6.1 |
|
25–44 years |
38 |
2.5 |
|
45+ years |
<10 |
- |
Note: Rates are not presented for age groups where there were fewer than ten cases. This is to ensure privacy and confidentiality is maintained.
First episode rheumatic fever hospitalisations, annual rate per 100,000 people, by Health District of Residence, 2024/2025
The following table details the number and rates of people being admitted to hospital with rheumatic fever for the first time in 2024/2025 by Health District of Residence.
|
Health District of Residence |
Numbers |
Rate per 100,000 |
|
Northland |
6 |
2.9 |
|
Waitematā |
26 |
3.9 |
|
Auckland |
23 |
4.6 |
|
Counties Manukau |
74 |
11.4 |
|
Waikato |
15 |
3.1 |
|
Lakes |
<5 |
- |
|
Bay of Plenty |
<5 |
- |
|
Hauora Tairāwhiti |
6 |
11.1 |
|
Taranaki |
<5 |
- |
|
Hawke’s Bay |
5 |
2.7 |
|
Midcentral |
<5 |
- |
|
Whanganui |
<5 |
- |
|
Capital and Coast |
11 |
3.3 |
|
Hutt Valley |
5 |
3.0 |
|
Wairarapa |
0 |
0.0 |
|
Nelson Marlborough |
<5 |
- |
|
West Coast |
0 |
0.0 |
|
Canterbury |
<5 |
- |
|
South Canterbury |
<5 |
- |
|
Southern |
<5 |
- |
Note: Rates are not presented for districts where there were fewer than five cases. This is to ensure privacy and confidentiality is maintained.
First episode rheumatic fever hospitalisations, annual rate per 100,000 people, by Health Region of Residence, 2024/2025
The following table details the number and rates of people being admitted to hospital with rheumatic fever for the first time in 2024/2025 by Health Region of Residence.
| Health Region of Residence | Numbers | Rate per 100,000 |
| Northern | 129 | 6.4 |
| Te Manawa Taki | 30 | 2.8 |
| Central - Te Ikaroa | 26 | 2.6 |
| Te Waipounamu | 9 | 0.7 |
Where to from here?
A five-year Rheumatic Fever Roadmap was launched in June 2023. The purpose of the Roadmap is to reset and refocus efforts around rheumatic fever and rheumatic heart disease prevention, identification and management, and sets out existing and new priority actions and opportunities for investment in the coming years.
The three focus areas of the Roadmap include:
- Whānau Ora – determinants of wellbeing and primary prevention.
- Tāngata Ora – quality health care and improved journey through the health system for those with rheumatic heart disease and rheumatic fever.
- Kōkiri Ngātahi – system readiness and change.
The Roadmap is available below.
Download: Rheumatic Fever Report 2024/2025 - XLSX, 602 KB
Rates and numbers are available for the New Zealand population, by ethnic group, age group and for health district.
Download: Rheumatic Fever Roadmap, 2023-2028 - PDF, 9.3 MB
The Rheumatic Fever Roadmap, 2023–2028 has been developed to reset, renew and amplify efforts in Aotearoa New Zealand to tackle rheumatic fever.