On this page
Management of eating disorders
This pathway is for the primary care management of individuals, both male and female, with a suspected eating disorder up to the age of 18 or those in the final year of high school. It does not give any guidance around the secondary care management of these conditions.
Assessment
Assessment
Identification and screening
Early identification and treatment of patients with an eating disorder is hugely valuable and makes a real difference in the outcome. Patients in this group have the highest mortality of any psychiatric disorder.
- Eating disorders can be difficult to detect in primary care.
- They will often be identified in educational settings from the school nurse or a teacher or from parental concerns.
- Individuals are often presented by parents or caregivers rather than themselves.
- Routine psychological assessment is probably the best way to pick up an eating disorder, and this can be done via a quick HEEADSSS assessment (see screening tools box)
- Target groups for screening:
- young women with low BMI compared with the age norm
- patients consulting with weight concerns who are not overweight
- women with menstrual disturbances or amenorrhea
- patients with gastro-intestinal symptoms, e.g. constipation, bloating, reflux
- patients with physical signs of starvation or repeated vomiting
- children with poor growth
- young people with type 1 diabetes and poor treatment adherence
- patients that present with dental problems e.g. gingivitis or toothache, may raise concerns if vomiting repeatedly.
- Higher risk groups for anorexia:
- young people who diet (x5 with moderate dieting, x18 with severe dieting)
- overweight people who suddenly lose a lot of weight
- boys who are into extreme exercise or body building.
- Useful questions:
- "Does your weight affect the way you feel about yourself?"
- "Are you satisfied with your eating patterns?
- "What do you think about your current weight and shape?
- "Have you cut out any food groups recently?"
- "Have you ever had anorexia?"
- "Has anybody ever suspected you have an eating disorder?"
- "Have you ever vomited or used laxatives, diuretics or enemas for weight loss or weight control?"
- Use the SCOFF questionnaire to help clarify any suspicion of an eating disorder – this is not a diagnostic tool but a guide:
- Do you make yourself sick because you feel uncomfortably full?
- Do you worry you have lost control over how much you eat?
- Have you recently lost > 1 stone (6.3kg) in a three-month period?
- Do you believe yourself to be fat when others say you are too thin?
- Would you say that food dominates your life?
(One point should be given for every “yes” answer; a score of more than or equal to 2 indicates a likelihood of anorexia nervosa or bulimia nervosa)
Screening tools
- HEEADSSS - Home, Education/Employment, Eating, Activities, Drugs & Alcohol, Sexuality, Suicide/ Depression,Safety - click here for some great online resources for training in this (external link).
- SCOFF questionnaire (see above).
Definitions
The diagnosis of an eating disorder will generally be made within the MDT team at a secondary level. The diagnostic criteria are stated here for reference only and should not be used over and above any clinical suspicion or concern regarding an individual’s presentation.
- Anorexia Nervosa (DSM V)
- Restriction of energy intake resulting in a significantly low body weight, or a less than minimally expected weight (based on age, sex or developmental trajectory)
- Intense fear of gaining weight; or persistent behaviour that interferes with weight gain, despite low weight
- Disturbance in body image; or persistent lack of recognition of the seriousness of the current low body weight
Sub-types: Restricting type, binge-eating/purging type
- Bulimia nervosa (DSM V)
- Recurrent episodes of binge eating (this involves eating an excessive amount of food in a discrete period of time AND a sense of lack of control)
- Recurrent inappropriate compensatory behaviours to prevent weight gain, such as vomiting, laxatives, diuretics, fasting or excessive exercise
- Frequency of at least once per week for three months
- Self-evaluation unduly influenced by body shape and weight
- Absence of anorexia nervosa
Subtypes: Purging type, non-purging type
- Avoidant or restrictive food intake disorder (ARFID)
- Eating or feeding disturbance with persistent failure to meet nutritional needs associated with either significant weight loss (or growth failure), significant nutritional deficiency, dependence on enteral/supplemental feeding or marked interference with psychosocial functioning
- Not explained by lack of available food or culturally sanctioned practice
- Absence of anorexia nervosa, bulimia nervosa or body image disturbance
- No intercurrent medical illness:
-
-
- Avoidant Restrictive Food Intake Disorder (ARFID) is a new diagnostic category in the DSM-5. It is defined as a persistent feeding or eating disturbance leading to avoidance of food, which results in significant weight loss or nutritional deficiency and/or impairment in psychosocial functioning. Unlike anorexia nervosa and bulimia nervosa, ARFID is not characterised by preoccupation with body shape and weight or by intentional weight loss behaviours. Instead, patients suffering from ARFID may be disinterested in food and eating with lack of appetite leading to slower rate of eating, eating smaller portions, and greater struggles around food.
- It is quite important to distinguish ARFID from picky eating, which is relatively common among children (20-30%) but only for a small subgroup of picky eaters their behaviour becomes more persistent, leading to either malnutrition and weight loss with medical complications similar to anorexia nervosa and/or impairment of psychosocial functioning. The avoidance of eating may also be caused by traumatic experiences related to consuming food, such as a personal or witnessed episode of choking, gagging or vomiting.
- Common Signs of ARFID
- Long history of ‘picky eating’ since childhood
- Lack of interest in food and eating
- Lack of appetite
- Slow rate of eating
- Eating smaller portions
- Greater struggles around food
- Avoidance of foods because of dislike of colour, texture, smell or taste
- Fear of choking, gagging or vomiting
- Gastrointestinal complaints like bloating, heartburn, nausea, constipation
- Weight loss and signs of malnutrition
- Avoidance of situations of social eating
-
- Binge eating disorder
- Recurrent episodes of binge eating
- Associated with symptoms such as eating more rapidly, feeling uncomfortably full, not feeling hungry, eating alone due to embarrassment and/or feelings of self-disgust
- Marked distress regarding binge eating
- Frequency of at least once per week for three months
- Absence of compensatory behaviours, anorexia nervosa and bulimia nervosa
- Other specified FED (OSFED)
- Eating disorders causing significant distress but not meeting criteria for other diagnostic categories.Examples include:
- Atypical anorexia nervosa – ‘normal weight anorexia nervosa’
- Bulimia nervosa (of low frequency and/or limited duration)
- Subthreshold binge – eating disorder
- Purging disorder
- Night eating syndrome
- Eating disorders causing significant distress but not meeting criteria for other diagnostic categories.Examples include:
History
Naturally, history will be targeted to the concerns raised. Useful areas to explore include:
- changes in behaviour around food
- general functioning at home and school
- changes in family and other relationships
- weight loss or gain, patterns or trends in BMI
- menstruation patterns
- specific symptoms – cold sensitivity, sleep disturbances, fainting or dizzy spells, dental problems, digestive problems, vomiting blood
- consider medical causes of weight loss, e.g. coeliac disease (see differential diagnosis).
Physical examination
- Height, accurate weight, BMI and BMI centile and previous measurements – This link has some good graphs. (external link)
- Lying and standing heart rate and blood pressure
- Body temperature
- Peripheral circulation – capillary refill, peripheral cyanosis, peripheral and sacral oedema
- Pubertal status
- Signs of binging or purging – including roughness on knuckle of index finger (Russell’s sign), enlargement of the parotid glands and dental erosion
- Evidence of deliberate self-harm – cuts or scars on the arms, thighs or abdomen
Investigations to consider
These may be done at the initial assessment but are not always helpful to do on an ongoing routine basis unless there is a valid reason to do so.
- Full blood count and ESR
- Urea and electrolytes, creatinine, calcium, magnesium, phosphate, random blood glucose
- Luteinising hormone, follicle-stimulating hormone, oestradiol (or testosterone, if male)
For young people with more advanced eating disorders or severe weight loss, add:
- Serum bicarbonate and pH on venous gas analysis (metabolic alkalosis may indicate vomiting)
- Liver function tests
- Thyroid function tests
- ECG – essential if any symptoms or signs of cardiac compromise, e.g. bradycardia, electrolyte abnormality, if patient has a BMI below 15kg/m3
Risk assessment
Patients with an eating disorder have a high risk in terms of their own safety and health. They have the highest mortality of any psychiatric disorder.
The factors involved in the assessment of risk in people with eating disorders include:
- medical risk
- psychological risk
- insight or capacity and motivation.
If there is immediate concern for safety it may be appropriate to contact the crisis team.
- Phone EBOP: 0800 774 545 or during business hours on 07 306 0154
- Phone WBOP: 0800 800 508 or during business hours 07 579 8329
If the patient requires compulsory assessment then they will need the Mental Health Act 1992. If this is needed then contact the duty authorised officer using the 0800 numbers above and they will provide the necessary forms.
Differential-diagnosis
Keep in mind that eating disorders may co-exist with other disorders.
- Consider other causes of weight loss if appropriate, such as:
- malabsorption, e.g. coeliac disease, inflammatory bowel disease
- diabetes mellitus
- glandular fever
- cancer
- substance or stimulant misuse
- infection, e.g. tuberculosis
- autoimmune disease
- endocrine disorder – e.g. hypothyroidism, addison’s disease.
- Other causes of amenorrhea include:
- pregnancy
- primary ovarian failure
- polycystic ovarian syndrome
- pituitary prolactinoma
- hypothalamic cause.
- Psychiatric differential diagnoses include:
- depressive disorder or episode
- obsessive compulsive disorder
- psychotic disorder
- Pre-pubertal children may show symptoms of eating disorder secondary to:
- emotional and behavioural disorders
- phobias
- refusal disorder.
Management
Management
1. Red flags and criteria for possible admission
- Please see admission criteria below for guidance around who might need to be admitted.
- This table is for those patients who are acutely unwell when you are assessing them. Please see the referral for specialist assessment below for guidance on referring patients in for outpatient assessment.
- If you have any concerns about an individual with possible eating disorders then in the first instance please contact the paediatrician on-call at either Tauranga or Whakatane.
- It is important to note that those individuals who are admitted often have poorer outcomes and so careful assessment of the need for admission is vital.
Admission criteria
|
Life-threatening weight loss
|
Acute medical complications of malnutrition
|
|
Acute food refusal |
Significant dehydration |
|
Hypoglycaemia |
Electrolyte imbalance
|
|
Physiological Instability
|
Arrhythmia |
|
Significant co-morbid psychiatric states
|
Failure to gain weight despite maximum outpatient treatment |
- 2. Food challenge
If there is some uncertainly as to whether the individual has an eating disorder:
- express concern around stated symptoms or behaviour
- highlight possible physical/psychological consequences of continued concerning food related behaviours
- encourage healthy behaviour around food and weight, use online resources
- establish a weight goal – around 200-500mg/week
- set up follow up in 2-3 weeks
- 3. Review: 2-3 weeks
- At this visit – weigh and assess symptoms or behaviours
- If there has been weight gain, change in behaviour and insight is good then agree to further monitoring with monthly review and weight for next 3 months.
- If no ongoing concerns, nothing further.
4. If continued concerns, refer for specialist assessment
Referral for specialist assessment guidelines
- Refer into Paediatrics or MICAMHS for any concerns around weight loss with no obvious cause as well as any concerns regarding an eating disorder.
- Early intervention is associated with improved prognosis.
- The individual will have a joint MICAMHS/Paediatric assessment which will usually take place within a few weeks of receiving the referral.
- Please include all previous height or weight parameters and pulse in referral as well as the relevant history, other examination findings and investigation to date.
Resources
Resources
For patients and carers
- EDANZ
This is a New Zealand based website with a huge wealth of resources to help support and provide information for people with eating disorders and their families. - Maudsley Parents
This website offers information on eating disorders and family-based treatment, family stories of recovery, supportive parent-to-parent advice, and treatment information for families who opt for family-based Maudsley treatment. - Families Empowered and Supporting Treatment of Eating Disorders
- Infant, Child and Adolescent Mental Health
Information and support for families and friends.
For providers
- Early identification and treatment of patients with an eating disorder is hugely valuable and makes a real difference in outcome. Patients in this group have the highest mortality of any psychiatric disorder
- If you have any concerns about a patient with a possible eating disorder then please discuss these with a specialist. (external link)
- EDANZ
- Infant, Child and Adolescent Mental Health
- Eating Disorders Recognition and Treatment UK
Acknowledgments
Acknowledgments
This pathway was developed in collaboration with the following people:
- Dr Kendell Crossen - SMO Paediatrician/Adolescent Specialist
- Dr Alison James - GP Liaison
- Amber Fletcher - Clinical Psychologist/Eating Disorder Liaison
Opiod substitution treatment (OST)
Background
Background
About substance abuse and drug dependency
Substance misuse is defined as use of a substance for a purpose not consistent with legal or medical guidelines, the substance having a negative effect on health or functioning and may take the form of drug dependence.
Dependence is defined as:
- a strong desire to take a substance, or difficulty in controlling its use
- the presence of a physiological withdrawal state
- tolerance of the use of the drug
- neglect of alternative pleasures
- persistent use of the drug despite harm to self and others.
Aims of OST
Aims:
- contribute to improving the health of patients as well as aspects of their personal and social functioning
- focus on improvements to quality of life such as education, employment, relationships with significant others
- reduce the spread of infectious diseases associated with injecting drug use, especially hepatitis B and C and HIV/AIDS
- reduce the mortality and morbidity resulting from the misuse of opioid drugs
- assist individuals to achieve successful withdrawal from opioid
- reduce episodes of illegal and other harmful drug use
- reduce crime associated with opioid use.
All aspects of service provision are aimed at reducing harm to the individual, the family/whanau and the community.
The Opioid Substitution Treatment offered should:
- suppress opioid withdrawal and craving
- not induce sedation or euphoria.
Maintenance doses are individualised to assist the patient to achieve their negotiated treatment goals.
Any increase or decrease in dose should be based on a clinical assessment. This clinical assessment might include a serum methadone level.
To achieve these aims the service focuses on:
- delivering person-centred, services that are both accessible and acceptable to patients
- maintaining a partnership approach with patients
- adopting a motivational rather than confrontational approach
- adopting prescribing practices that are evidence and strengths based
- supporting planned withdrawal from methadone or buprenorphine/naloxone when appropriate
Patient confidentiality and privacy are maintained in accordance with relevant legislation and patient consent is obtained in line with the requirements of the Code of Health and Disability Services Consumer Rights Act 1996.
*See Section 1.1 Objectives of OST page 4-5 of " New Zealand Practice Guidelines for Opioid Substitution Treatment 2014 (external link)"
How does OST shared care work?
Why transfer to GP Shared care?
OST aims to support patients to live as normal a lifestyle as possible within the parameters of treatment. GP shared care has the benefits of;
- Instigating more comprehensive health care for patients.
- Allowing services to focus on patients in need for intensive specialist input.
- Improving social integration by normalizing patients treatment.
The phases of treatment provide a patient pathway based on recovery principles. A person may or may not move sequentially through the phases from high intervention to low intervention, but as with any recovery process, may experience periods of higher intervention (re-stabilisation or a return to specialist maintenance) as part of their recovery.
Underpinning the practices and policies of BOPAS is local and international research which demonstrates the effectiveness of Opioid Substitution Treatment (OST). Treatment provided by BOPAS is delivered within a framework of sound medical practice, accepted standards, approved guidelines and legal requirements. BOPAS seek to ensure that methadone or buprenorphine/naloxone is prescribed and dispensed in a clinically responsible manner.
Roles and responsibilities
- The BOPAS lead medical officer as authorising medical officer retains overall responsibility for patients on the GP Shared Care programme.
- GP authorization is based on a shared care model of service delivery. BOPAS provide specialist support and can always be accessed for advice or assistance. Renewal of authorization is contingent upon prescribing practices remaining consistent with BOPAS policy and regular review with lead clinician.
- For roles and responsibilities of the patient, GP and BOPAS, please see documents below:
- Bay of Plenty Addiction service GP Shared Care Agreement (external link).
- Authority for a general practitioner to prescribe controlled drugs for the treatment of addiction (section 24(2) (d) MODA (external link)).
- For information regarding writing of scripts and the storage etc. of script pads please click here. (external link)
See Section 8 OST in Primary Care page 60-62 of "New Zealand Practice Guidelines for Opioid Substitution Treatment 2014 (external link)"
Assessment
Assessment
Instability indicators:
- problematic, harmful or hazardous use of alcohol or other drugs
- engages in or supports criminal activity
- signs of intoxication at clinic or pharmacy
- evidence of intravenous injecting
- irregular dosing
- poor attendance at appointments
- avoidance of urinalysis or blood tests
- behavioural problems such as aggression
- frequently requests changes to dispensing
- requests to replace lost or stolen doses
- any co-existing mental or physical health problems are difficult to treat or are not well managed.
- *see Section 1.2 Roles of Specialists OST Services page 5 of "New Zealand Practice Guidelines for Opioid Substitution Treatment 2014 (external link)"
Stability indicators:
- defined and progressing towards treatment goals.
- no problematic, harmful or hazardous use of alcohol or drugs.
- no evidence of criminal activity.
- responsible management of takeaways.
- schedules and attends appointments.
- rarely requests changes to dispensing.
- social stability as evidenced by relationships with others, stable and healthy housing, employment/occupation.
- any co-existing mental or physical health problems are well managed.
- participates in primary health care.
- complies with programme requirements.
Recommended reviews:
- Appointments:
- Initially the patient will see his/her GP every 28 days when a new script is needed. This is recommended to occur for at least 3 months when the patient is new to your practice. Where there is an established relationship with the patient or there are other indications for less frequent appointments this can be negotiated between the GP, patient and Addiction Liaison Clinician (from the BOPAS service).
- After this initial time the patient must be seen by the GP once every 3 months for a review. The patient usually collects their script from the GP, practice nurse or receptionist at their review and in the two months between the three monthly appointments.
- Three monthly review
- Click here to access the GP Shared Care Patient Review checklist (external link)
- Not attending appointments
- If a patient consistently does not attend appointments, the GP may refrain from writing any further scripts until the patient is seen or may write a short-term interim prescription until a new appointment can be scheduled. The GP should also contact the case manager and or the Addiction Liaison Clinician.
- GP - Six Monthly Information Forms
- The Addiction Liaison Clinician will contact your practice at least every six months to update information. Please provide any additional information you may wish to raise at this time or any time between contacts. It is essential for BOPAS to have current information for continued GP prescribing authorisation.
Management
Management
Visit the drug or drug-related issues pathway (external link) or prescribing issues pathway (external link)
BOPAS Contacts
Bay of Plenty Addiction Service (BOPAS)
Postal address:
Kowhai House
Tauranga Hospital
Cameron Road
Private Bag 12024
Tauranga 3143
Opening hours: Monday to Friday, 8.30am to 5pm
- email: bopas@bopdhb.govt.nz
- phone reception: 07 579 8391
- phone crisis team (after hours): 07 579 8329 or 0800 800 508
Concurrent issues
Pain Management
Acute pain:
- Mild to moderate acute pain can usually be effectively managed with simple analgesics (including mild opioid medications) and/or other appropriate medications.
- Opioid maintenance patients with acute severe pain usually require higher doses of opioid agonists than non-opioid tolerant patients in order to achieve adequate pain relief. (Many receive inadequate analgesia for acute severe pain).
- In the event an OST patient is hospitalised their GP prescriber will need to liaise with the hospital staff to ensure continuation of methadone or buprenorphine/naloxone in hospital, cancellation of the prescription at the community pharmacy and the resumption of prescribing at the community pharmacy on discharge. BOPAS can assist as required.
Chronic pain:
- Chronic pain in Opioid maintenance patients should be managed in the same way as it is for other patients.
- Methadone or buprenorphine/naloxone as prescribed for maintenance treatment may provide partial relief for some chronic pain.
- BOPAS advises consultation with a specialist pain management service or BOPAS medical officer before considering the regular prescribing of opioid medication for the management of chronic pain.
- Note: Long term methadone treatment can saturate and dull opioid receptors leading to increased patient pain levels as the body tries to compensate for inhibited pain recognition (hyper-analgesia; increased sensitivity to pain secondary to long-term blockade of opiate-based pain receptors)
- *See Section 6.6; 6.6.1; 6.6.2 Management of Acute and Chronic Pain page 49 of "New Zealand Practice Guidelines for Opioid Substitution Treatment 2014 (external link)"
Pregnancy:
- There are several health problems during pregnancy that should be discussed including:
- General nutrition.
- Risks of anaemia.
- Alcohol and nicotine consumption.
- Oral hygiene and dental health.
- Complications from chronic infection related to injection practice.
- Antenatal and postnatal mental health problems.
- Advice should be given regarding potential complications of pregnancy associated with drug use:
- Premature delivery.
- Low birth weight.
- Placental abruption.
- Neonatal abstinence syndrome.
- Opioid detoxification in pregnant women:
- Should be undertaken with caution; and
- In the second trimester with small frequent reductions − however, expert opinion suggests that a patient should be free to choose to initiate detoxification at any stage of pregnancy, provided her circumstances and her ability to cope are taken into consideration.
- Partial splitting of the dose may also be considered for stable pregnant patients in the latter half of pregnancy in order to avoid the necessity for increase in the dose, especially for those on doses below 60mg. A single daily dose should be reinstituted following delivery.
- Note: A small number of women become fast metabolizers of methadone or buprenorphine/naloxone in pregnancy. Where this is suspected, obtain trough and peak serum methadone levels and discuss with the BOPAS before instituting split dosing. These women are at greater risk of destabilization in pregnancy and timely assessment and management can prevent this.
Breastfeeding:
- In general, it is safe to breastfeed while a mother is taking methadone as long as there are no other factors that would make breastfeeding unsafe, such as using illegal drugs or using certain prescription medications. Methadone is found in breast milk, but only a small amount gets passed along to the baby.
- There are many benefits to breastfeeding for both the mother and her baby including:
- Breast milk has important nutrients that will help baby grow and may help prevent infection.
- Babies who are breastfed are generally more healthy and don't have to visit the doctor as often as babies who are fed formula.
- Breastfeeding helps the mother and her baby bond.
- Breastfeeding may help baby cope with withdrawal symptoms.
- Although there is no official statement saying that mothers cannot breastfeed if they are taking methadone, it would be wise to discuss this with the specialist service to learn more about it.
- *See Section 6.7 Management of Pregnant and Breastfeeding Women page 52-56 of "New Zealand Practice Guidelines for Opioid Substitution Treatment 2014 (external link)"
Concurrent Medical Conditions
HIV/hepatitis B and C
- Issues for the GP managing a patient on Opioid Substitution Treatment (OST) are:
- testing for HIV, Hepatitis A, B and C (including Hep C PCR RNA test)
- preventing infection/transmission
- monitoring LFTs in those with chronic Hepatitis B and C
- offering treatment for hep C, or refer for specialist treatment where required
- offering Hepatitis A and B vaccination to those who are HAV and HBV antibody negative.
Chronic liver disease
- Patients with chronic liver disease on long-term opioid maintenance usually do not require alterations in their dose. However, if there is an abrupt change in liver function they may require dose adjustment. The development of jaundice is also a sign that the liver may not be able to metabolize methadone or buprenorphine/naloxone at the normal rate.
- Where there is significant impairment it is suggested that the methadone serum level is checked every 2 to 3 months to ensure that it is not rising due to impaired metabolism of methadone. Seek the advice of BOPAS or a specialist gastroenterologist if there are concerns.
Respiratory disorders
Methadone or buprenorphine/naloxone is a respiratory depressant and care should be taken in prescribing methadone or buprenorphine/naloxone to patients with these disorders.
Epilepsy
Note that carbamazepine, phenytoin and phenobarbitone interact with methadone (see methadone or buprenorphine/naloxone interactions section).
Mental health disorders
Note that antidepressant and antipsychotic medications may interact with methadone or buprenorphine/naloxone (see methadone or buprenorphine/naloxone interactions).
Resources
Resources
For providers
- GP Shared Care manual [DOCX, 998 KB]
- GP Shared Care 3 monthly OST patient review checklist [PDF, 88 KB]
- GP Shared Care agreement [PDF, 131 KB]
- Authority for GP to prescribe controlled drugs for the treatment of addiction [PDF, 64 KB]
- NZ practice guidelines for Opioid Substitution Treatment [PDF, 1 MB]
- National Opioid Substitution Treatment Training Programme [PDF, 582 KB]
- Best practice article on Opioid Addiction October 2014 (external link)
- BOP community pharmacy feedback form [PDF, 274 KB]
- Auckland opioid treatment service website and resources (external link)
- Regional Maori health services cultural practice manual [PDF, 439 KB]
For patients
- OST and you - A guide to Opioid Substitution Treatment
About the Tauranga Opioid Substitution Treatment service (OST)
The Tauranga Opioid Substitution Treatment service (OST) is one of the services offered by Bay of Plenty Addiction Service (BOPAS) that is part of Mental Health and Addiction Services, Bay of Plenty District Health Board (BOPDHB).
This pathway contains information and guidelines for General Practitioners authorized by BOPAS OST to prescribe methadone or buprenorphine/naloxone to patients in the GP Shared Care Programme. BOPAS OST intends that this information will assist in the provision of a quality, safe, professionally delivered OST Service that meets the needs of patients, their family/whanau, and the wider community. GPs and their staff are encouraged to consult with the Addiction Liaison Clinician or the Lead Clinician at BOPAS OST working in a shared-care partnership model.
BOPAS OST provides services for the management of opioid dependency from a harm reduction philosophy, supporting people towards recovery, relative to each individual and his or her own circumstances.
The OST programme is in accordance with:
The BOPAS Service manages the admission, stabilisation and specialist maintenance phases of OST treatment. Patients may then be assessed as meeting criteria for the GP Shared Care Programme where their OST is integrated with their primary health care provider who is authorised by BOPAS on a three-monthly (6-monthly with permission from the MOH) basis to prescribe methadone or buprenorphine/naloxone.
Acknowledgements
Acknowledgements
This pathway was developed in collaboration with:
Service |
Name |
|---|---|
|
Mental Health SMO Tauranga |
Sue Mackersey* |
|
WBOPPHO GP |
Jocelyn Heard* |
|
GP Liaison Nurse - OST |
Andy Walford |
|
WBOPPHO GP |
Tony Farrell |
|
Clinical Team Leader, BOP Addiction Service |
Paula Abbey |
|
Clinical Lead BOPAS |
Sally Whitelaw |
|
Mental Health SMO |
David Chaplow |
|
Community Pharmacist |
Rebecca Lukey |
|
P&F |
Lesley Watkins |
|
Pain Service |
Vicky Beveridge |
|
Program Manager Bay Navigator |
Caroline Davy |
*Pathway lead
OST prescribing issues
Background
Background
About opioid substitution treatment prescribing issues
The Tauranga Opioid Substitution Treatment service (OST) is one of the services offered by Bay of Plenty Addiction Service (BOPAS) that is part of the wider Mental Health and Addiction Services at Health New Zealand Bay of Plenty.
This pathway contains information and guidelines for general practitioners authorized by BOPAS OST to prescribe methadone or buprenorphine/naloxone to patients in the GP Shared Care Programme. BOPAS OST intends that this information will assist in the provision of a quality, safe, professionally delivered OST Service that meets the needs of patients, their family/whanau, and the wider community. GPs and their staff are encouraged to consult with the Addiction Liaison Clinician or the Lead Clinician at BOPAS OST working in a shared-care partnership model.
BOPAS OST provides services for the management of opioid dependency from a harm reduction philosophy, supporting people towards recovery, relative to each individual and his or her own circumstances.
The OST programme is in accordance with:
The BOPAS Service manages the admission, stabilisation and specialist maintenance phases of OST treatment. Patients may then be assessed as meeting criteria for the GP Shared Care Programme where their OST is integrated with their primary health care provider who is authorised by BOPAS on a three-monthly (6-monthly with permission from the MOH) basis to prescribe methadone or buprenorphine/naloxone.
Prescribing issues
Prescribing issues
-
What to do when GP on leave or absent
- GPs are urged to appoint a locum or practice partner to prescribe methadone or buprenorphine/naloxone to their authorised patients in their absence and to ensure that BOPAS, locum/practice partner and other practice staff are informed of this.
- The BOPAS OST, Addiction Liaison Clinician is also available to support the locum/practice partner.
- Should the GP plan to be away for longer than three months he/she needs to contact the Addiction Liaison Clinician so that BOPAS OST service can arrange authorization(s) for the locum or a practice partner (as required by Medsafe) and provide training and extra support.
-
Prescribing for holidays or travel
- Public holidays (Please contact BOPAS for support as required):
- The GP is responsible for identifying when a patient's dispensing day/s fall on a public holiday and should annotate the prescription accordingly, i.e., write instructions for any change in dispensing required due to closure of the pharmacy. If space is limited use an additional sheet and attach it to the prescription. The Addiction Liaison Clinician can assist with a generic holiday schedule that can be adjusted to suit individual needs.
- It is preferred that no more than three consecutive takeaway doses are approved at any one time, except in the case of public holidays where pharmacies are not providing a service or in exceptional circumstances. In such cases 1 (one) additional takeaway dose (i.e., a total of four takeaway doses) may be prescribed for a patient providing the Patient, the Addiction Liaison Clinician and the GP are confident that it is a safe arrangement.
- Patient holidays (within New Zealand):
- The GP, with Addiction Liaison Clinician support, is responsible for organising alternative dispensing arrangements for patients on holiday. See transfers between pharmacies.
- Patients should provide the GP with adequate notice of holidays.
- Travel overseas:
- GPs are advised to contact the Addiction Liaison Clinician for information and assistance with arranging overseas travel as soon as they receive a request from a patient. It is preferred that arrangements be made for the patient to be dispensed methadone or buprenorphine/naloxone via a programme in the country of destination.
- Note: If the patient needs to travel with methadone or buprenorphine/naloxone doses they will require an exportation letter (explains dose and form (usually tablets) prescribed and the dates the medication is prescribed for).
- Adequate notice (usually several weeks) is required to make these arrangements. More time may be required when a patient is travelling to more than one destination or where other complexities exist. There are a number of countries where OST is not available and/or where importation of methadone or buprenorphine/naloxone is illegal. In an emergency situation overseas travel may be arranged more quickly but this does not apply to all countries of destination.
- *See Section 5.7 Travelling Overseas with Opioid Substitution Medication page 40 of “New Zealand Practice Guidelines for Opioid Substitution Treatment 2014 (external link)"
- Public holidays (Please contact BOPAS for support as required):
-
Take away arrangements
- Methadone or buprenorphine/naloxone Takeaway Arrangements:
- A takeaway dose of methadone or buprenorphine/naloxone is any dose that is not consumed under observation at the dispensing pharmacy.
- Takeaway arrangements in the GP Programme continue to be based on clinical safety and within the National Practice Guidelines.
- Note: The National Practice Guidelines recommend that methadone or buprenorphine/naloxone should be observed to be consumed at the pharmacy or other dispensary on at least three non-consecutive days per week.
- Variance: Where the authorised GP and the patient assess that less frequent dispensing is appropriate, this is notified to Addiction Liaison Clinician for BOPAS OST team review. Once the OST service supports the requested change, a new authorisation would need to be prepared to reflect these changes. A copy will be sent to the GP, the pharmacy and the Ministry of Health.
- Following the review any variance from the above policy needs to be documented and referenced in relation to the indicators of stability and instability. Evidence such as proof of employment might be required to support requests for less frequent observation.
- Note:
- Every client in New Zealand must consume observed at least once weekly.
- GPs are advised to refrain from making any changes to takeaway arrangements during the first 3 to 6 months in the GP programme to enable time to fully assess the patient and their safety with further takeaways.
- *See Section 5.1 Takeaway Doses page 36 of "New Zealand Practice Guidelines for Opioid Substitution Treatment 2014 (external link)"
- Methadone or buprenorphine/naloxone Takeaway Arrangements:
-
Requests for replacement doses
- Replacement Doses: BOPAS OST policy is not to replace doses under any circumstances e.g., lost, stolen, spilt, damaged, retched.
- If in exceptional circumstances that can be verified (i.e., by a police report, eyewitness by professional), the GP may (after discussion with the BOPAS OST service) offer to assess the patient 48 hours or more after their last dose was consumed and if there are signs of opioid withdrawal then part of subsequent doses may be replaced. When requests are made for replacement doses the GP should review the person's takeaway arrangements and notify the case manager and or Addiction Liaison Clinician.
- BOPAS policy is to replace 50% of a vomited methadone dose when the patient vomits within approximately 30 minutes of consuming the dose, the vomiting was witnessed by a professional and the replacement is clinically appropriate. (e.g., pregnancy)
- As buprenorphine/naloxone is absorbed sublingually, there is no need to replace doses after vomiting.
- If a second replacement dose for vomiting is requested within a short time, or there are regular requests for replacement doses, no further replacement doses should be authorized until the patient has been assessed by the GP and any underlying cause for the vomiting assessed and treated.
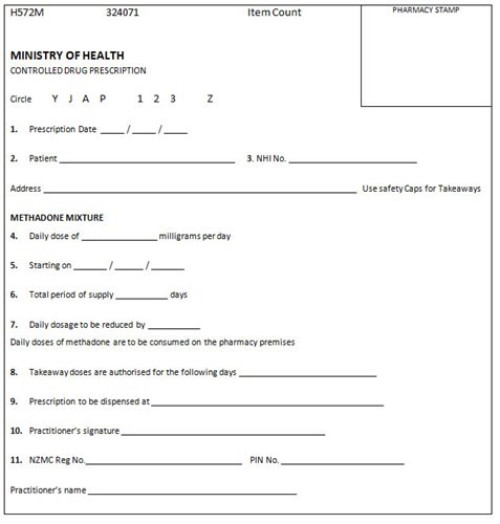
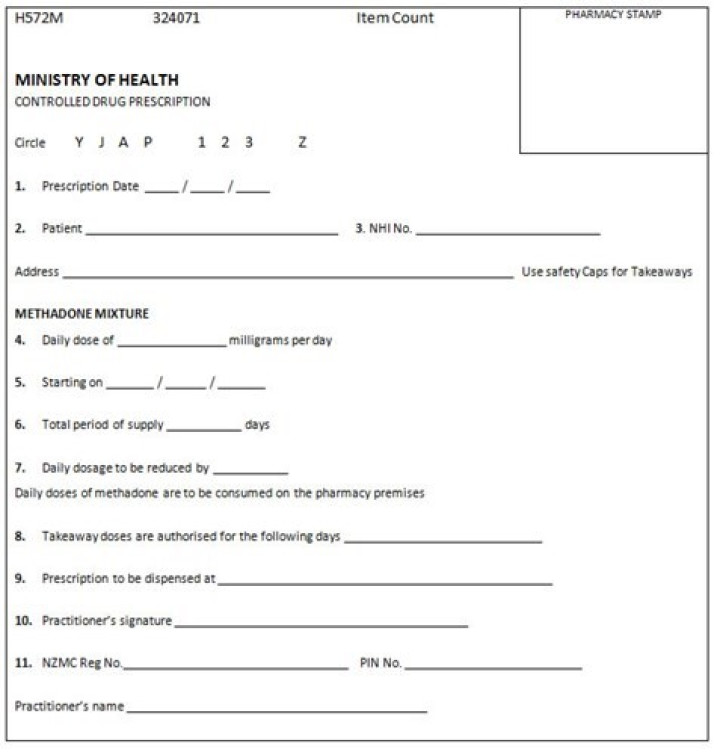
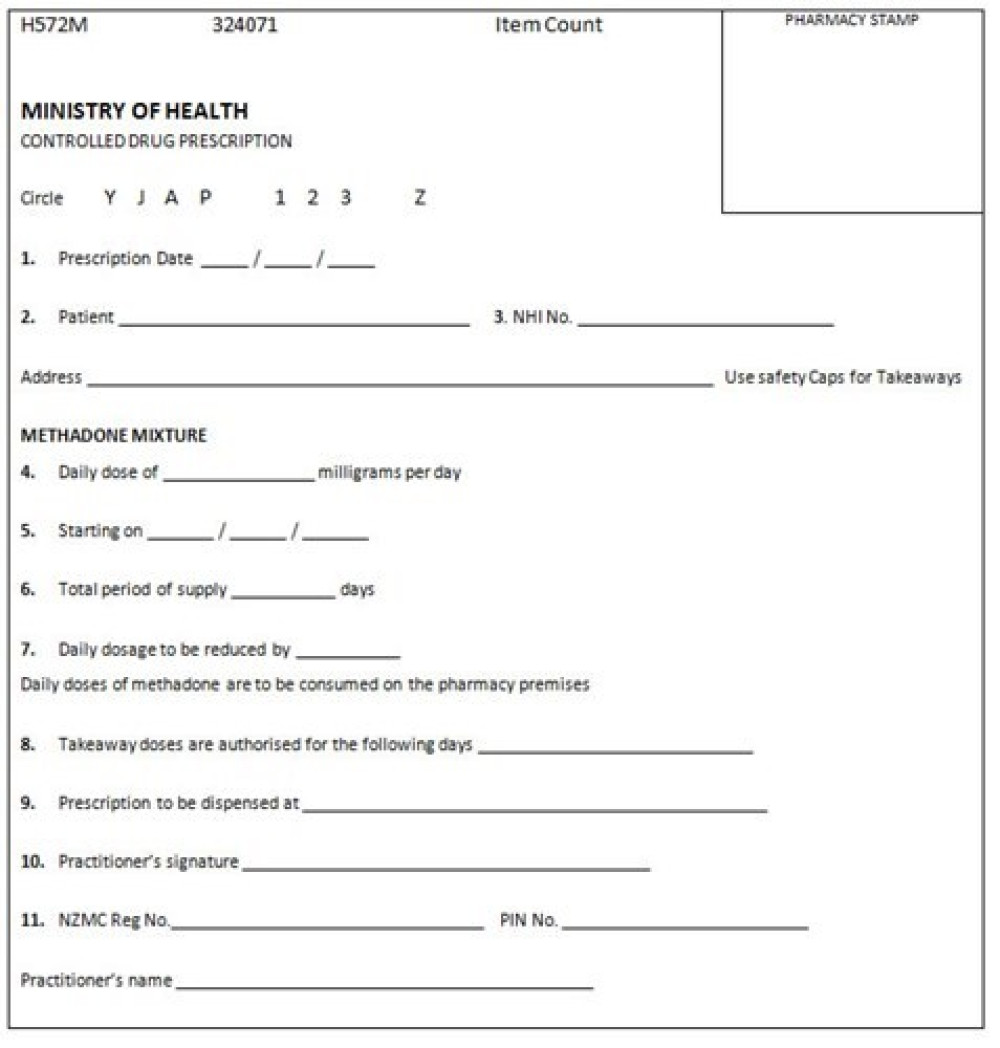
- All replacement doses must be prescribed on a new H572M prescription and must be consumed in the pharmacy.
- Note: repeatedly seeking replacement dose is likely instability indicator.
- *See Section 5.3; 5.3.1; 5.3.2 Replacement Doses page 38 of “New Zealand Practice Guidelines for Opioid Substitution Treatment 2014 (external link)"
-
Agents acting on behalf
- Agents Collecting on Behalf of a Patient: A GP can authorise an agent to collect OST on behalf of a patient in extraordinary circumstances where the patient is unable to attend the pharmacy e.g., when they are house-bound due to illness. Circumstances necessitating the authorization of an agent must be verified with the patient and the agent.
- Authorization of an agent is limited to a maximum of 3 doses of methadone or buprenorphine/naloxone dispensing.
- Authorization must be made in writing and faxed to the appropriate pharmacy and include:
- Name and address of the agent.
- Type of identification provided by agent.
- Number of doses the agent is authorised to collect.
- Signature of the authorising GP
- The authorised agent must provide suitable identification.
- Note: The GP must feel confident that the authorised agents can responsibly manage and administer the methadone/ buprenorphine/naloxone.
- Discussion about safety of takeaways is essential e.g., storage away from children, no replacement of lost or stolen doses.
-
How to write a prescription
- Writing a methadone H572 controlled drug prescription
- The use of H572M controlled drug prescription forms is restricted to prescribing methadone for patients under the authority conferred by Section 24(2) (d) Misuse of Drugs Act 1975 (i.e., where BOPAS has authorised a prescriber for a specific patient). The form is not used for prescribing of methadone to other patients in other circumstances (e.g., pain relief for a non-BOPAS client); in these cases, the general H572 controlled drug prescription is used.
- H572 Prescription example and instructions (external link)
- Ordering
- These CD pads are requested 3-6 monthly by GPs based on their current number of authorised patients.
- Orders are faxed to the Ministry of Health using the approved order form (refer to Forms section). On receipt of the pads, sign the enclosed verification of delivery form and fax to the Ministry of Health as soon as possible.
- Ministry of Health contacts
- MedSafe Office - ph. 09 441-3670
- Storage
- These CD pads must be stored in a secure place as for other CD prescription pads. You are advised to keep the receipt for the pads as a record of the prescription pad numbers.
- Theft of prescription forms
- If the prescription numbers are known, inform the Ministry of Health MedSafe office. If the prescription numbers are unknown, inform the Ministry of Health and request the prescription numbers of the pads recently sent to the practice. Inform the MOH MedSafe office of the numbers.
- Ceasing to prescribe
- Notify the Ministry of Health that you no longer require these pads.
- Receipt of excess pads
- Notify the Ministry of Health that you no longer require these pads. Destroy or return any unused pads to the Ministry of Health
- Writing a methadone H572 controlled drug prescription
-
Split Methadone or Buprenorphine/Naloxone dosing
- For the vast majority of patients adequate stability can be achieved on a once daily dose of methadone or buprenorphine/naloxone.
- Patients in GP shared care are unlikely to require a change to split dosing, unless in exceptional circumstances.
- Partial splitting of the dose may also be considered for stable pregnant patients in the latter half of pregnancy in order to avoid the necessity for increase in the dose, especially for those on doses below 60mg. A single daily dose should be reinstituted following delivery--See OST and Pregnancy (external link)
- Note: A small number of women become fast metabolizers of methadone or buprenorphine/naloxone in pregnancy. Where this is suspected, obtain trough and peak serum levels and discuss with the BOPAS before instituting split dosing. These women are at greater risk of destabilization in pregnancy and timely assessment and management can prevent this.
- Split dosing may also be considered for stable patients in the latter part of a planned withdrawal from methadone or buprenorphine/naloxone (usually at doses of 30mg or less) in order to reduce pre-dose withdrawal symptoms and to increase the likelihood of successful completion of withdrawal from methadone or buprenorphine/naloxone. This needs discussion with and authorisation by the OST service.
- Split dosing may be in exceptional circumstances considered for stable patients to better manage physical pain symptoms.
- Split dosing(including the proportions of each dose) requires the approval of the BOPAS
- *See Section 5.6 Split Methadone Doses page 40 of "New Zealand Practice Guidelines for Opioid Substitution Treatment 2014 (external link)"
-
Transfers between pharmacies
- The case manager and or addiction liaison clinician may assist you with this.
- Otherwise:
- Establish with the patient which dispensing pharmacy in the area is suitable and confirm with the pharmacy that they are able to dispense to the patient.
- Cancel the script at their existing pharmacy.
- Write a new script for the new pharmacy and fax it to them if necessary.
- Contact the Addiction Liaison Clinician to request that an 'Introduction to Pharmacy' letter with a photo ID is sent to the new pharmacy.
- The patient will be required to provide photo-ID at the new pharmacy.
-
Transfer to another OST Programme
- Contact the BOPAS OST with details about the proposed new location of the patient and request assistance with the transfer.
- Note: Waiting times for transfer to other OST programmes vary considerably throughout the country.
- Where a patient is stable the treatment service at the new location may agree to the transfer of the patient directly to a GP authorised by that service and the transfer may be achieved more quickly. Alternatively, out of area prescribing may be arranged until such time as the local OST service is able to take them onto their programme. However, during this interim period the patient should return to be seen at least 3 monthly by their prescribing doctor. The Specialist OST service will not be able to authorise an out of area GP.
- *See Section 7.1 Transferring between Specialist Services page 57 of "New Zealand Practice Guidelines for Opioid Substitution Treatment 2014 (external link)"
-
Managing missed doses
- The pharmacy should notify you if the patient misses any doses. Three or more consecutive missed doses as under National protocols the patient must be reassessed by the BOPAS OST service, before dispensing can resume. They need to be seen and assessed as to whether it is safe for them to resume dispensing the usual dose or whether they require a dose decrease due to reduced tolerance. Opioid tolerance rapidly changes, so several days without opioids can significantly alter tolerance to prescribed OST.
Resources
Resources
For providers
- GP Shared Care manual [DOCX, 998 KB]
- GP Shared Care 3 monthly OST patient review checklist [PDF, 88 KB]
- GP Shared Care agreement [PDF, 131 KB]
- Authority for GP to prescribe controlled drugs for the treatment of addiction [PDF, 64 KB]
- NZ practice guidelines for OST [PDF, 1 MB]
- National OST training programme [PDF, 582 KB]
- Best practice article on opioid addiction October 2014 (external link)
- BOP community pharmacy feedback form [PDF, 274 KB]
- Auckland opioid treatment service website and resources (external link)
- Regional Maori health services cultural practice manual [PDF, 439 KB]
For patients
Acknowledgments
Acknowledgments
This pathway was developed in collaboration with:
Service |
Name |
|---|---|
|
Mental Health SMO Tauranga |
Sue Mackersey* |
|
WBOPPHO GP |
Jocelyn Heard* |
|
GP Liaison Nurse - OST |
Andy Walford |
|
WBOPPHO GP |
Tony Farrell |
|
Clinical Team Leader, BOP Addiction Service |
Paula Abbey |
|
Clinical Lead BOPAS |
Sally Whitelaw |
|
Mental Health SMO |
David Chaplow |
|
Community Pharmacist |
Rebecca Lukey |
|
P&F |
Lesley Watkins |
|
Pain Service |
Vicky Beveridge |
|
Program Manager Bay Navigator |
Caroline Davy |
*Pathway lead