On this page
Waikato Hospital has been offering cytoreductive surgery combined with heated intraperitoneal chemotherapy (HIPEC) since 2008. Over the years, they have successfully completed performed over 370 procedures. This complex technique is carried out by a specialized team that includes surgeons, anaesthetists, oncologists, theatre nursing staff, perfusionists, perioperative nursing care, dieticians, and pathologists.
Waikato is one of only six hospitals in Australia and New Zealand that perform cytoreductive surgery with HIPEC. They are also part of the ANZ Peritoneal Malignancy Collaboration, which supports research and advancements in this field across Australasia.
Indications
Waikato Hospital provides cytoreductive surgery with heated intraperitoneal chemotherapy for the following indications:
- Appendiceal tumours with peritoneal metastases including Pseudomyxoma peritonei
- Colorectal cancer with isolated peritoneal metastases (PCI <15) and highly selected cases of colorectal cancer peritoneal metastases with synchronous low-volume extra-peritoneal metastases
- Malignant peritoneal mesothelioma
- Highly selected cases of gynaecological malignancy, at the request of gynaecological oncology specialists
Referral to Multi-Disciplinary Meeting discussion to consultation
Referrals and enquiries can be sent to:
You need to complete an MDM form. Please email us for the form.
The referring clinician or an appropriate delegate presents in person or via Microsoft Teams. The deadline for submitting discussion materials is Wednesdays 12pm before the Multi-Disciplinary Meeting (MDM). If the appropriate information or pathological specimens are not available in time for the discussion, it will need to be deferred.
Discussions occur on fortnightly on Fridays at 8am and the outcome of the discussion will be emailed to the referring clinician on the following Monday. Please ensure all relevant notes, laboratory results and scans are made available through email and the Waikato PACS system (radiology) for review prior to MDM.
Clinic appointments will be scheduled within 2 to 4 weeks of referral, based on the urgency required for surgery. The expected time frames for surgery depend on the indication, volume of disease, and the patient's symptoms. If your patient's condition is worsening or you have any other concerns, please let us know via the email above so we can prioritize their treatment.
Treatment is also available in the private sector.
From first specialist assessment (FSA) to surgery
If possible, patients are scheduled for a pre-anaesthetic assessment clinic on the day of their consultation in Waikato.
In some cases, we may request an anaesthetic assessment at the referring hospital.
Patients are booked for admission to Waikato Hospital the day prior to surgery, and will usually be visited by the treating team that day (surgeon, anaesthetist, colorectal CNS, charge nurse, stoma therapist.)
Nationally agreed treatment targets are 4-6 weeks for high-grade cancer such as colorectal adenocarcinoma, appendiceal carcinoma and mesothelioma, and 2-4 months for pseudomyxoma peritonei.
Staging
The staging investigations required for work up depends on the indication, but would typically include:
- tumour markers (CEA, CA19-9, CA125)
- diagnostic/staging laparoscopy with biopsy (or image guided core biopsy)
- assessment of PCI
- full staging CT scan
- colonoscopy.
An FDG-PET scan and staging laparoscopy (where feasible) are essential for patients with colorectal cancer.
Follow up guidelines
After surgery, patients are discussed at a pathology MDM where the pathology is discussed and the slides are reviewed. In some instances, adjuvant chemotherapy is recommended and a letter will go to the referrer to request a review from oncology at the referring institution.
Surveillance guidelines are otherwise 4 monthly CEA, CA19-9 and CA125, except for colorectal cancer where CEA alone is tested.
CT scans are suggested at 1, 2, 3 and 5 years. with additional CT scans at 7 and 10 years for pseudomyxoma peritonei.
Recurrences may be suitable for repeat surgery with HIPEC, and we would appreciate a referral for discussion if a patient we have treated has had recurrent disease diagnosed.
Research and audit
Waikato maintains a prospective database of patients for audit and research, to ensure that the highest level of care can be provided to our patients. Waikato is also part of the ANZ Peritoneal Malignancy Collaboration, contributing to research and the development of consensus guidelines for the management of peritoneal disease. A link to our data and outcomes can be found below:
- Long-term survival following cytoreductive surgery and hyperthermic intraperitoneal chemotherapy in Waikato, Aotearoa New Zealand: a 12-year experience. (external link)
- Cytoreductive surgery and hyperthermic intraperitoneal chemotherapy in New Zealand: peri- operative outcomes and service development over a decade. (external link)
Information for patients
Cytoreductive surgery with heated intraperitoneal chemotherapy is offered to patients with disease localised within the peritoneal cavity. The primary site of origin could include the appendix, colon or rectum, ovary or malignant mesothelioma.
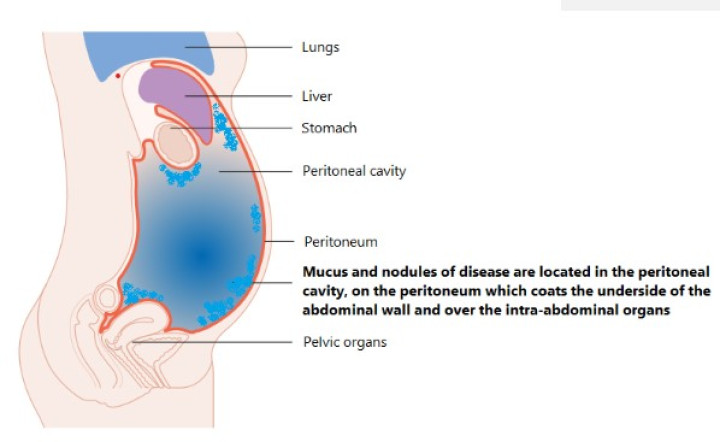
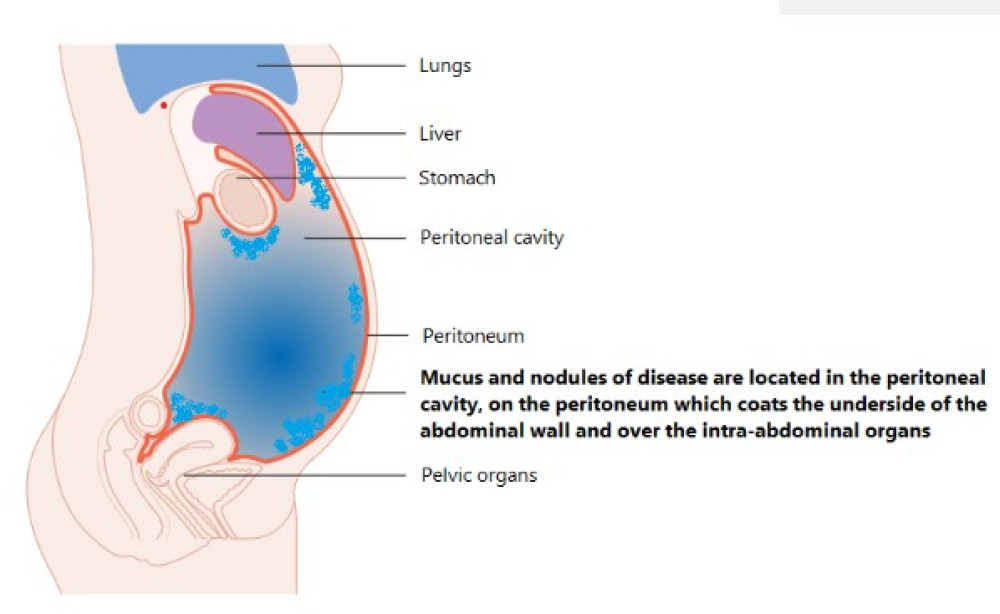
The peritoneal cavity is a space within the abdomen that is typically insufflated when one has a laparoscopy.
The peritoneum is a layer of tissue which covers the underside of the abdominal wall, diaphragm and coats the organs. Disease within the peritoneal cavity tends to sit on the peritoneum and abdominal organs, rather than infiltrate into them and spreading to the lymph glands or elsewhere in the body, thereby allowing its removal.
The aim of cytoreductive surgery is to remove all visible disease. To do this, the peritoneum is stripped away and any organs which contain disease are removed. This may include the spleen, part of the stomach, omentum, gallbladder, large intestine, uterus and ovaries. A small amount of the small bowel may be able to be removed but not all, and disease located around the main trunk of blood supply to the liver can also be difficult to remove in entirety. Once all visible disease is removed, heated chemotherapy is instilled into the abdominal cavity by a perfusionist for 90 minutes, which kills any remaining viable tumour cells.
To date, Waikato has performed over 370 procedures and the operation is performed by one of 5 surgeons, often working in pairs. The majority of patients have been treated for pseudomyxoma peritonei of appendiceal origin, but an increasing number are offered surgery for colorectal cancer where there is limited peritoneal disease.
Surgery is a major undertaking and requires a specialised multidisciplinary team, versed in the procedure, post-operative care and interpretation of pathology and follow up. The operation takes 9 hours on average to complete and patients are transferred to the high dependency unit post operatively for 2 days. Recovery in hospital is expected to take up to around 2 weeks, before patients are discharged home or transferred to the referring hospital. Full recovery to baseline function can take many months.
Complications can occur and whether minor or major, occur in 30 to 40% of people. Complications from the chemotherapy are rare, and have not been seen in our cohort of patients. In some instances, a stoma is required and may be permanent or temporary. For women of childbearing age, it is important to let your specialist know if you are planning to have a family, as there is an opportunity to be referred to a fertility specialist.
Surgery is very daunting, especially for those living outside of Waikato. There are options for accommodation for family, the details of which can be provided. We also have patients who are more than happy to talk about their past experiences, and this can be particularly helpful for some people.
For any queries, please email: peritonectomy@waikatodhb.health.nz
Team
Mr Simione Lolohea
Colorectal, General and Laparoscopic Surgeon, Endoscopist
Mr Ralph Van Dalen
Colorectal, General and Laparoscopic Surgeon, Endoscopist
Mr Linus Wu
Colorectal, General and Laparoscopic Surgeon, Endoscopist
Mr Jasen Ly
Colorectal, General and Laparoscopic Surgeon, Endoscopist
Mr Nick Smith
Colorectal, General and Laparoscopic Surgeon, Endoscopist
Mr Jesse Fischer
Colorectal, General and Laparoscopic Surgeon, Endoscopist
Jay Haden
Clinical Nurse Specialist - Colorectal Cancer
Caro Stahell
Clinical Nurse Specialist - Colorectal Cancer